Antigen
n., plural: antigens
[ˈæntɪdʒən]
Any of the various substances that when recognized as non-self by the immune system will trigger an immune responseImage Credit: NIH Image Gallery. An electron micrograph of a dendritic cell, an antigen-presenting cell, interacting with T cells via its endogenous antigens on its cell surface.
Table of Contents
Antigen Definition
What is an antigen? A simple definition is that an antigen refers to any substance that triggers an immune response. This response is intended to naturally protect the body from harmful entities, such as disease-causing microbes and neoplastic growth. In humans, some of the immune responses activated by the presence of antigens are antibody formation, induction of cell-mediated immunity, complement activation, and development of immunological tolerance. Not all antigens are able to elicit antibody production or cellular immunity. Those that are capable of activating B or T lymphocytes and by themselves stimulate and serve as the target of an immune response are referred to as immunogens.
Antigen Structure
Antigens are mainly polysaccharides or protein molecules. Nucleic acids and lipids become antigenic only when combined with a polysaccharide or protein molecule. When the antibody is formed, it reacts with the hapten only without interacting with the carrier molecule. Penicillin is a hapten since the drug itself is not antigenic, however, in some individuals, penicillin combines with a specific protein in the host where the resulting complex stimulates an immune response.
Types of Antigens
There are three fundamental types of antigens according to their origin:
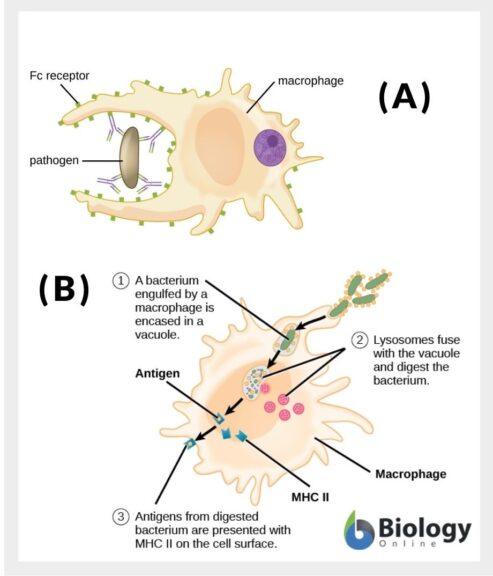
- Exogenous antigens are antigens that are nonself, meaning they are not a cellular constituent of the body but have gained entry into the body nonetheless. They came from the outside and have entered into the body of the organism, e.g. by inhalation or ingestion. When recognized, they could be taken up by antigen-presenting cells (e.g. macrophages, dendritic cells). Examples of exogenous antigens: allergens, proteins from transplanted tissues and organs, substances on the surface of foreign cells, toxins, and other foreign particles.
- Endogenous antigens are antigens produced from within a normal cell and then presented outside of the cell on the cell surface. Examples: antigens presented by cells that have become infected by bacteria or viruses, blood group antigens on the cell surface of erythrocytes (e.g. H antigen on RBCs, A antigens, and B antigens), HLA or histocompatibility leukocyte antigens.
- Autoantigens are a special type of endogenous antigens. They are mistakenly identified by the immune cells as nonself and therefore are acted upon by the immune system. These antigens are normally produced by the cells of the body. However, certain factors (e.g. environmental or genetic) caused the immune cell to identify them as foreign and therefore attack the cell. This is what occurs in autoimmune diseases. Examples of autoantigens are nucleoproteins, and nucleic acids. (Microbiologyinfo.com, 2015)
Antigens may also be classified based on their immune response. As already cited earlier, an immunogen (typically a protein or a polysaccharide) is an antigen that can elicit an immune response by itself, meaning it can trigger a lymphocyte to act against it. In contrast, an antigen that cannot elicit an immune response on its own is referred to as a hapten. It needs another substance — a carrier molecule such as albumin or globulin for instance — before it can trigger an immune response. Compared with an immunogen (with a molecular weight of more than 10,000), hapten has a lower molecular weight (less than 10,000). Tolerogen is an antigen that instead of inducing an immune response it suppresses, thereby causing immune tolerance. It binds to the antigen receptor of the lymphocytes to suppress them.
Antigen Examples
As already mentioned above, there are different types of antigens. They may be classified according to their origins, such as exogenous antigens, endogenous antigens, and autoantigens. Different sources of antigens can induce various immune reactions as exogenous antigens are processed and presented in MHC class II whereas endogenous antigens are presented in MHC class I.
Exogenous antigens can be a part of microorganisms, transplanted organs or tissues, or allergens. They are presented in MHC class II.
An endogenous antigen is an antigen synthesized inside the cell and it is usually present as a result of viral or parasitic infection. Endogenous cells are also present on altered cells such as tumor cells or infected cells.
The endogenous antigen is recognized by cytotoxic T-cells (CTL) on MHC class I so CTL can attack infected or altered cells through the release of perforin that forms pores in the cell membrane leading to its death.
Autoantigen is a self-antigen; it is a natural component of the cell that is recognized by the immune system leading to an autoimmune disease. Normally, self-antigens do not trigger immune responses since they are naturally present in the body, however, in autoimmune diseases, altered immune cells are triggered by the natural self-antigens.
Antigen Detection
The antigen may be detected by the body through exposure to a B-cell receptor (BCR) in humoral immunity or to a T-cell receptor (TCR) in cellular immunity. These cell receptors are highly antigen-specific. BCRs are responsible for detecting extracellular or free antigens whereas TCRs are responsible for detecting intracellular antigens.
Antigens can be a component of an invading pathogen such as cell wall, fimbriae, flagella, capsule, bacterial toxins, viral coats, or on the surface of other pathogens. Pathogenic antigens are commonly known as pathogen-associated molecular patterns (PAMPs).
PAMPs are recognized by the host when PAMPs attach to a receptor of the family of toll-like receptors (TLR). The resulting complex serves as a warning trigger for the host of an invading organism.
Antigenic molecules or cells stimulate very specific immune responses when they attach to BCR. They stimulate the formation of antibodies specific to the antigen in order to eliminate the invading antigen.
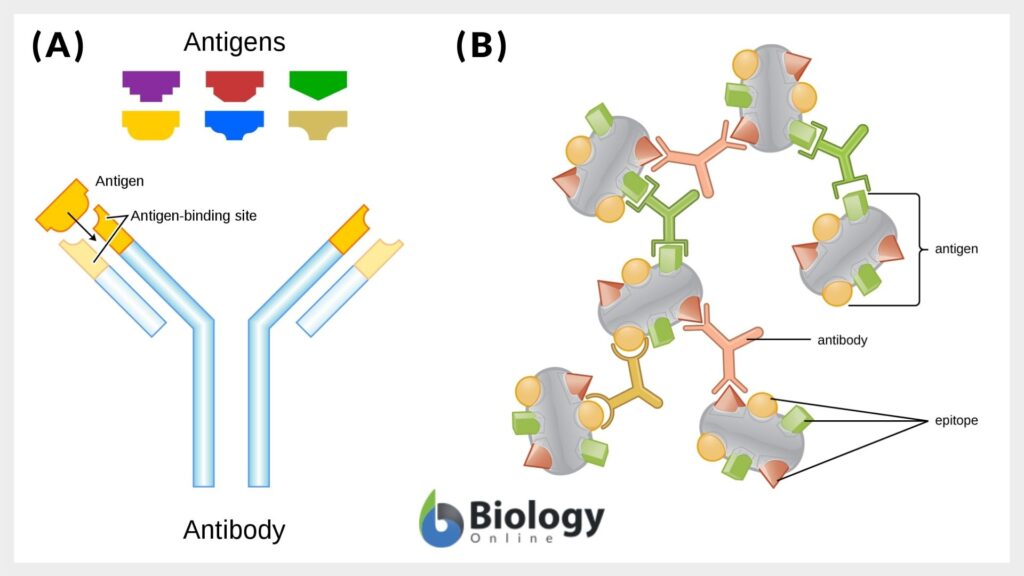
T-dependent antigens require the help of T-helper cells to produce antibodies against these antigens. Components of an antigen called epitopes (or antigenic determinants) are the regions where the antigen and the antibody interact with each other on the pathogenic cell. The Y-shaped antibodies recognize and attach to each specific antigen at their two identical antigen-binding sites. Human antibodies usually have only two antigen-binding sites so they are bivalent.
Other antigens are non-microbial, such as those found on the surface of transplanted organs or tissues, blood cells surface, pollens, serum proteins, or egg white. These non-microbial antigens are not associated with pathogens, however, they can trigger the adaptive immune response.
Antigens present on the surface of human red blood cells are used for the classification of blood groups such that some blood groups have antigens on the surface of the red blood cells while other groups lack certain antigens. Antigens on red blood cells are non-immunogenic under normal conditions. Rather, they participate in chemical reactions, help in the attachment of other molecules, aid in the transportation of various molecules into and out of the cell and maintain the cell structure. The table below shows the different human ABO blood groups and the IgM antibodies present in each.
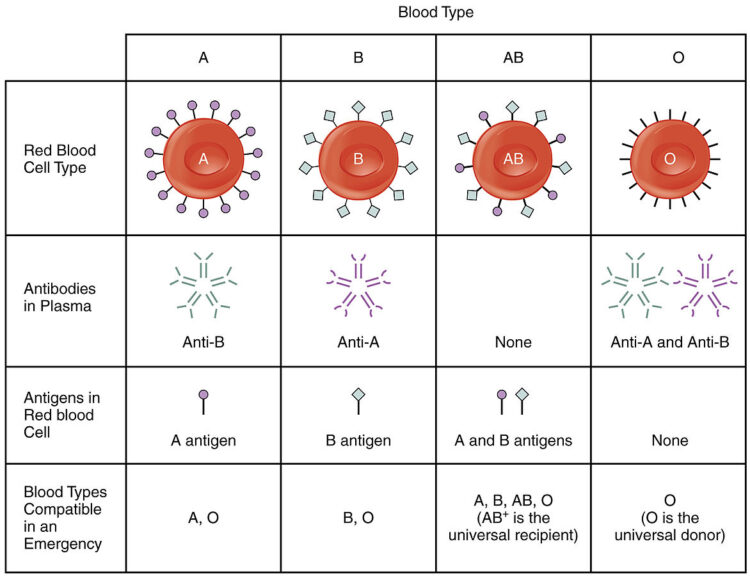
Blood group antigens will trigger an immune response if, for instance, a human receives a blood transfusion from a donor with a different blood group antigen. The body recognizes the transfused blood as foreign cells in the body, consequently initiating an immune response. Antibodies attack the transfused blood antigens and this may lead to serious adverse health effects; therefore, the recipient’s and the donor’s blood groups should be matched before blood transfusion or organ donation in order to avoid the stimulation of this immune response.
Antigen Processing and Presentation
Self-antigens are a natural component of the body cells. B and T cells that cannot recognize self-antigens are eliminated by apoptosis whereas normal B and T cells ignore self-antigens as means of autoimmunity suppression. However, damage, infection, or impaired apoptosis can trigger the immune response against self-antigens leading to an autoimmune disease.
Intracellular pathogenic antigens that infect cells do not come in contact with the circulating antibodies so their antigens are not presented. Intracellular immunity can help in eliminating intracellular pathogens and abnormal cells such as cancer cells.
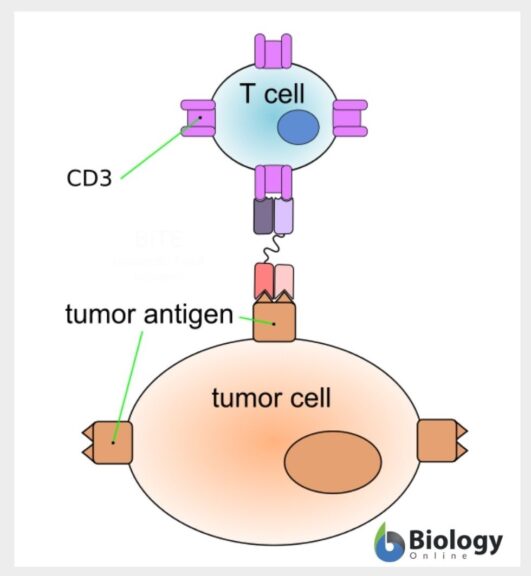
T-cells are responsible for intracellular antigens encountering, they are most abundant in both lungs and gastrointestinal tract where most intracellular antigens enter the body. Gastrointestinal antigens can also be taken by M cells found on the intestinal wall; they transfer these antigens to antigen-presenting cells or lymphocytes in order to be recognized by antibodies.
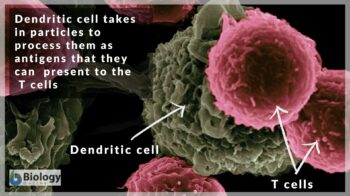
Antigen-presenting cells are cells that engulf and present antigens to other immune cells to encounter the antigen. The antigen processing and presentation process is mediated by Major histocompatibility complex (MHC) class I and MHC class II found on the surface of the antigen-presenting cells, antigen-presenting cells include B-cells, dendritic cells, and macrophages.
After antigen engulfment, dendritic cells and macrophages migrate to lymph nodes to present antigens to T-cells in lymph nodes. T-cells specific for this antigen, then, migrate to the antigen site to encounter it.
Antigen-antibody Complex Formation
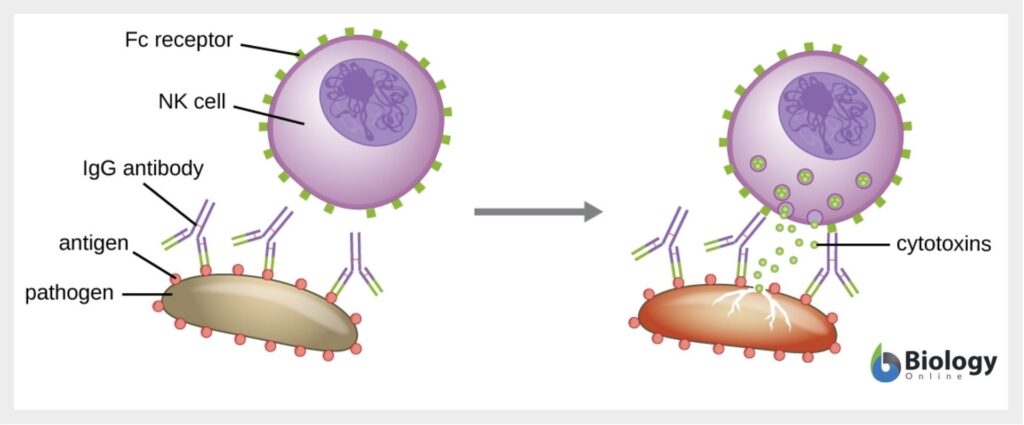
The antibody attachment to the antigen is not practically harmful to the antigen. However, it triggers pathogenic destruction by other immunological mechanisms such as agglutination, complement activation, neutralization, opsonization, and antibody-dependent-cell-mediated cytotoxicity.
In agglutination, antibodies attach to a great number of antigens so they clump together. As a result, the number of infectious organisms decreases to be easily phagocytosed. Complement activation is a process where antibodies trigger the activation of the complement system that causes inflammation and microbial lysis. For neutralization, antibodies surround the pathogen preventing its attachment to the host cell. They can neutralize bacterial toxins in a similar manner. In opsonization, the antigen-antibody complex or the complement proteins can improve pathogen ingestion by phagocytic cells. Antibody-dependant cell-mediated cytotoxicity is somehow similar to opsonization where antibodies coat the antigen, however, in antibody-dependant cell-mediated cytotoxicity, the target cell is destroyed by natural killer cells or eosinophils that remain outside the target cell without ingesting it. Some pathogens can evade the immune response against antigens by altering their antigens in a process known as antigenic variation.
Diagnostic Immunology
Antibodies are so specific to each antigen that they can even differentiate between two isomers of amino acids in the antigen’s nucleic acid sequence. Therefore, antigen-antibody complex formation is used to determine and differentiate between different types of antigens using monoclonal antibodies.
Soluble antigens can be determined by precipitation reaction. The antigen-antibody complex aggregates form a lattice that indicates the presence of a specific antigen. Conversely, insoluble antigens or soluble antigens that adhere to a particle can be aggregated together to form distinct aggregates in a reaction called agglutination reaction.
Because antibodies can neutralize the harmful effect of bacterial exotoxins or prevent the adhesion of some viruses to the host cells, this reaction is, therefore, used as an indication of the presence of these viruses.
The virus is added to the patient’s serum containing red blood cells. If hemagglutination was not observed, this means that the neutralizing antibodies are present, inhibiting the viral action.
Fluorescent-antibody techniques are used to detect either the presence of a certain antigen or antibodies that were previously attached to antigens using a labeled antibody. Fluorescent-dye-labeled antibodies fluoresce when exposed to ultraviolet light as viewed using a fluorescence microscope. The most commonly used immunological test is known as Enzyme-Linked Immunosorbent Assay (ELISA) which determines the presence of a specific antigen or of antibodies against a specific antigen. Since it is available as a prepared kit and the detection process is usually automated, ELISA is used by the public as a pregnancy test.
Try to answer the quiz below to check what you have learned so far about antigens.
References
- Lackie, J. (2007). The dictionary of cell and molecular biology. Amsterdam Boston: Elsevier. p.213.
- MicrobiologyInfo.com. (2015, May 17). Antigen- Properties, Types and Determinants of Antigenicity. Microbiology Info.Com. https://microbiologyinfo.com/antigen-properties-types-and-determinants-of-antigenicity/
- Tortora, G. J., Funke, B. R., & Case, C. L. (2015). Microbiology: an introduction. Pearson Higher Ed.
- Davies, D. R., Padlan, E. A., & Sheriff, S. (1990). Antibody-antigen complexes. Annual review of biochemistry, 59(1), 439-473.
- Blood group antigens – Genetics Home Reference – NIH. (2020, August 17). Retrieved September 22, 2020, from https://ghr.nlm.nih.gov/primer/genefamily/bloodgroupantigens
- Self antigens. In: Moreland L.W. (eds) Rheumatology and Immunology Therapy. Springer, Berlin, Heidelberg (2004) . Retrieved September 22, 2020, from https://doi.org/10.1007/3-540-29662-X_2408
©BiologyOnline.com. Content provided and moderated by BiologyOnline Editors.