Bone matrix
n., plural: bone matrices (or bone matrixes)
[ˈboʊn ˈmeɪtɹɪks]
Definition: Extracellular matrix of bone
Table of Contents
Bone Matrix Definition
Bone matrix refers to the matrix component of bone tissue. It provides the structural framework and mechanical support for bones, especially as it provides a site where new bone tissues are deposited during bone growth, remodeling, and repair. The bone matrix is made up of organic and inorganic components. The organic component includes collagen fibers and ground substance. The inorganic component refers to the inorganic bone salts, mainly the hydroxyapatite. The collagen fibers give bone tissues their flexibility and tensile strength. Minerals that impregnate the bone matrix, such as calcium and phosphate, in turn, help make the bone hard and rigid.
Let us understand further the definition of the bone matrix along with the other parts that make up the bone tissue of the body as well as its role in bone mechanical properties (strength, rigidity, resilience, and a degree of flexibility). In this module, we will also look at the bone matrix composition (both organic and inorganic components) and its functions.
Watch this vid about bone matrix:
Biology definition:
The bone matrix is the intercellular substance of the bone tissue. It is that part of bone tissue comprised of organic and inorganic substances. The bone matrix is also regarded as the extracellular matrix of bone tissues and forms most of the bone mass. The matrix of the bone includes both organic and inorganic components. The organic component of the bone matrix is primarily made up of collagen and ground substance whereas the inorganic component is made up of inorganic bone salts, mainly hydroxyapatite, and other minerals.
Synonym: osteoid
Composition Of Bone Matrix
What is bone matrix made of?
The bone matrix is composed of organic and inorganic components. In human bones, the organic components constitute approximately 35-40% whereas the inorganic components contribute about 60-65% of the bone’s dry weight, implicating that the inorganic matrix of bone is greater than the organic parts of bone matrix.
The composition of the bone matrix is as follows:
Organic bone matrix components
The collagen and ground substance are the primary organic components of the bone matrix. Other organic components are other bone matrix proteins, noncollagenous proteins, proteoglycans, and growth factors.
- Collagen: Collagens are the predominant type of protein in the bone matrix. They are of two types: fibrillar and nonfibrillar.
- Fibrillar type: Examples of fibrillar collagen are Type I collagen, Type III collagen, and Type V collagen. The primary type of collagen though is Type I collagen. Type I collagen is an important component as it plays various roles:
- ✓ Type I collagen provides tensile strength that allows the bone to resist stretching and bending, and support the body weight.
- ✓ Type I collagen gives bones a degree of flexibility, especially to withstand forces without breaking.
- ✓ Type I collagen provides a scaffold for the deposition of mineral crystals during the mineralization of the bone, especially during bone formation, bone remodeling, and bone regeneration or repair.
- ✓ Type I collagen interacts with the cells in the matrix, which is crucial in bone homeostasis.
- Nonfibrillar collagen: Apart from fibrillar types, nonfibrillar collagens are also present albeit in relatively smaller amounts than fibrillar types. Examples of nonfibrillar collagen in bone matrix are Type IV and Type XIII. Although they do not occur as fibers, they are important nonetheless. They contribute to the overall maintenance of the integrity and function of bone tissue. In particular, Type IV collagen, which is a major component of basement membranes (specialized extracellular matrices) of bones that form the bone lining cells that cover bone surfaces. Type XIII collagen is present in the bone matrix and has been implicated in cell adhesion and cell signaling processes.
- Fibrillar type: Examples of fibrillar collagen are Type I collagen, Type III collagen, and Type V collagen. The primary type of collagen though is Type I collagen. Type I collagen is an important component as it plays various roles:
- Ground substance: Just as the other ground substance in other parts of the body, this nonfibrillar amorphous material fills the space. In the bone matrix, it fills the space between the collagen fibers and hydroxyapatite crystals. The ground substance contains glycoproteins, proteoglycans, and glycosaminoglycans. It helps maintain the structural integrity of the bone tissue.
- Other organic components: Apart from the collagen and ground substance, other organic components of the bone matrix are as follows:
- Osteocalcin, also known as bone Gla protein, is a vitamin K-dependent bone matrix protein. Osteocalcin function: bone mineralization and calcium ion binding
- Osteopontin is a phosphoprotein involved in the regulation of the interaction between the cells and the bone matrix during bone remodeling or bone renewal.
- Bone Sialoprotein is another phosphoprotein involved in cell adhesion, signaling, and bone mineralization.
- Matrix Gla Protein is a vitamin K-dependent protein involved in inhibiting the calcification of soft tissues.
- Proteoglycans are organic molecules composed of proteins and glycosaminoglycans. In the bone matrix, they are involved in the regulation of bone mineralization and maintaining the structure of the extracellular matrix.
- Glycoproteins are proteins with carbohydrate chains. They have adhesive properties and play a role in cell-matrix interactions.
- Growth Factors, such as transforming growth factor-beta (TGF-β), fibroblast growth factors (FGFs), and bone morphogenetic proteins (BMPs), play a role in regulating bone cell activities, including cell proliferation, cell differentiation, cell migration, and new bone formation.
These organic components interact with the inorganic components to make the bone tissue dynamic and resilient.
Inorganic components
The inorganic components of the bone matrix are mainly the mineralized hydroxyapatite along with the small amounts of other inorganic minerals and ions. Some of the inorganic components in the bone matrix are as follows:
- Hydroxyapatite: Hydroxyapatite [chemical formula: Ca10(PO4)6(OH)2] is a calcium phosphate biomineral. It is in crystalline form and occurs as the predominant component of the bone matrix (significantly greater than the other bone matrix components, including Type I collagen, which contributes to approximately 35% of the bone’s dry weight).
- Other minerals: some of them are as follows …
- Calcium (Ca2+) ions are an essential component of hydroxyapatite crystals and are crucial for bone mineralization.
- Phosphate (PO43-) ions are also part of the hydroxyapatite bone matrix and are necessary for bone mineralization.
- Magnesium (Mg2+) ions also have a vital role in bone mineralization and in regulating calcium levels.
- Sodium (Na+) ions are involved in maintaining the body’s electrolyte balance.
- Potassium (K+) ions help maintain the acid-base balance in the bone.
Formation of the Bone Matrix and Osteogenesis
A bone includes both living and nonliving material. The bone matrix is described as a non-living component of the bone tissue (osseous tissue). This is because the bone matrix is a mineralized substance outside the cells. Yes, apart from the matrix of bones, the bone is composed of cellular elements as well.
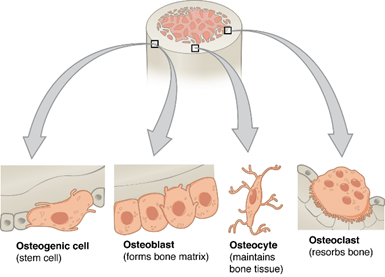
The different types of cells you will find in bone tissue are as follows:
- Osteoprogenitor cells (osteogenic cells or osteoprogenitors) are stem-like cells with the capacity to divide mitotically. They are actively involved in bone growth and repair. They are initially located in the periosteum (outer fibrous layer of bone), endosteum (inner cellular layer of bone), and bone marrow.
- The cells that secrete the organic components of the bone matrix are called osteoblasts. They are the primary bone-forming cells. Osteoblasts are capable of mitosis, too, and thereby can give rise to other osteoblasts. However, many of them also came from osteoprogenitors that have differentiated into osteoblasts (which have a relatively lower capacity for mitosis).
- Cells that break down the bone tissue (bone resorption) are called osteoclasts.
- Osteoblasts that have matured and eventually become more associated with bone remodeling are called osteocytes.
Osteoblasts and other bone cells have specific receptors on their cell surfaces, such as integrins, which allow them to adhere to the bone matrix.
Quick question! Which among those types of bone cells is responsible for the deposition of organic and inorganic substances that make up the bone matrix?
If you’re thinking of osteoblasts, you are correct!
The bone matrix is produced by osteoblasts; these bone cells release deposits for the bone matrix. Osteoblast is a cell that stores calcium in bone by making bone matrix. Nevertheless, osteoblasts along with the other bone cells work to form a dynamic and constantly remodeling tissue to maintain bone function and homeostasis.
Bone formation, also called osteogenesis, occurs throughout life. The bone is continually remodeled, with the old bone being resorbed and then replaced with the new one.
Let’s see the different steps of bone formation (osteogenesis or ossification) wherein the formation of the bone matrix (osteoid formation) is one of the crucial steps.
- Mesenchymal cell condensation and osteoprogenitor formation: this is when the mesenchymal cells (undifferentiated stem cells) at the site of bone development condense and then differentiate to become osteoprogenitor cells.
- Osteoblastogenesis: this is the process wherein the osteoprogenitor cells differentiate into osteoblasts.
- First, the osteoprogenitor cells from the periosteum (outer fibrous layer of the bone), endosteum (inner cellular layer of the bone), or bone marrow (the soft, spongy tissue found within the hollow spaces of bones) are recruited into the site of injury upon the activation of signaling molecules and growth factors.
- Second, the osteoprogenitor cells undergo cell division (proliferation) to increase their number.
- Third, some osteoprogenitor cells will undergo bone cell differentiation to transform into specialized cells — osteoblasts — a process called osteoblast differentiation.
- Osteoid collagen formation and bone matrix mineralization: this is when the bone matrix forms.
- Initially, osteoblasts produce and secrete protein fibers in bone (mainly Type I collagen) to form the osteoid. Osteoid is laid down to serve as the scaffold upon which the subsequent mineralization occurs.
- Later, they deposit calcium and phosphate ions onto the collagen scaffold. This forms the hydroxyapatite mineral into the matrix, which gives the bone its hardness and rigidity. So while the osteoblasts continue to deposit collagen and other proteins, they also facilitate the deposition of inorganic minerals onto the collagen framework.
- Osteocyte formation: Because of the deposits released, the osteoblasts are eventually “trapped” or “entombed” in the mineralized matrix. At this point, they become mature bone cells, osteocytes, which are the primary bone cells responsible for bone remodeling.
- Bone remodeling: this process involves the coordinated work of osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells).
Bone Matrix Function
The bone matrix is an essential component of the osseous tissue that makes up a bone. It is, in fact, one of the features that differentiate bones from cartilage. While both tissues are connective tissues, an osseous tissue matrix is composed of mostly Type I collagen and hydroxyapatite crystals. Conversely, cartilage has a different extracellular matrix composition. Cartilage matrix consists mainly of Type II collagen and proteoglycans that make cartilage rather flexible and not as hard or rigid as the bone. The bone matrix, thus, is key to the mineralization of bones, which is an essential feature of the fundamental component of the skeletal system.
The mineralized tissue of the bone consists of the following layers:
(1) Compact bone (or cortical bone) tissue, which is the outer, hard layer of the bone
(2) Cancellous bone (or spongy bone) tissue, which is the inner, spongy layer of the bone
See the long bone-labeled diagram below.
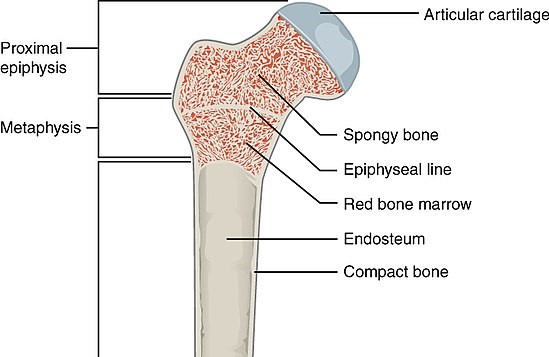 | 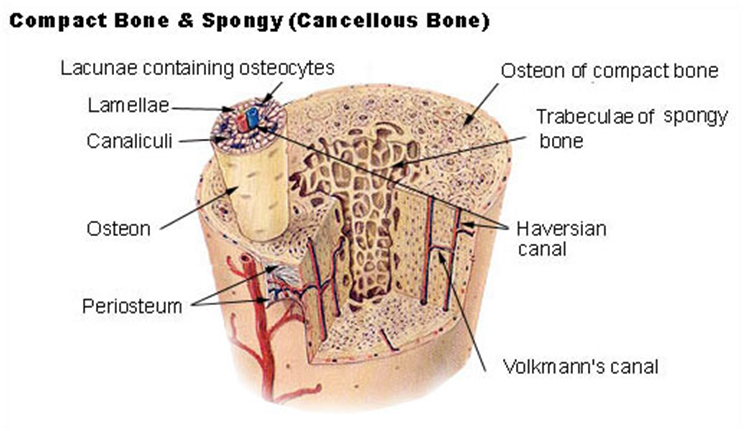 |
| Figure 2: Normal bone composition diagrams. Take note of the lamellar bone organized into layers of mineralized bone matrix. Credits: OpenStax College (left) and SEER (right). Left: bone labeled diagram: internal structure of a human bone. Note that the bone consists of compact and spongy bone layers. Right: bone histology diagram. Notice the structure of bones: the outer surface of the bone is covered by the periosteum, which is a layer consisting of fibrous connective tissue lined with osteoprogenitor cells. The compact bone is made up of an osteon (Haversian system), which is the primary structural and functional unit of a compact bone. The osteon is made up, in turn, of concentric layers of calcified matrix (lamellae) of dense bone tissue around the central Haversian canal — the canal that runs through the core of each osteon and contains blood vessels, lymphatic vessels, nerves, and loose connective tissue). Conversely, the spongy bone is made up of plate or rod-shaped lamellae called trabeculae. | |
There are notable differences between the compact bone matrix (also known as cortical bone) and the spongy bone matrix (also known as trabecular bone or cancellous bone). See the table below for a comparison.
Table 1: Compact bone matrix vs. Spongy bone matrix | ||
|---|---|---|
| Features | Compact bone matrix | Spongy bone matrix |
| Bone structure and morphology | Highly organized and dense. There are tightly packed osteons (Haversian systems) arranged in concentric circles around a central Haversian canal. The osteon is composed of organized layers of lamellae (thin sheets) of bone matrix. | Has a more porous and latticed structure with interconnecting trabeculae (thin columns) of bone tissue. The spaces between the trabeculae are filled with bone marrow. The trabecular lamellae are part of the bone matrix that appear as thin, parallel layers of bone tissue that make up the structural framework of spongy bone. |
| Distribution | Outer layers of bones | Inner regions of bones |
| Bone density | Much denser and heavier | Has a lower density due to its porous nature, thus, lighter |
| Composition | Contains predominantly Type I collagen fibers and inorganic minerals, such as hydroxyapatite crystals (calcium phosphate) | Contains Type I collagen fibers, but it has a lower mineral content compared to the compact bone matrix. The trabeculae are composed of lamellae, but they are not as organized as in compact bone. |
| Function | The highly organized structure of the compact bone matrix provides excellent mechanical strength and rigidity, making it suitable for withstanding mechanical stresses and supporting the weight of the body. | The porous structure of the spongy bone matrix allows for a lightweight design that provides support while reducing the overall weight of the bone. It is also involved in blood cell production within the bone marrow spaces. |
Apart from providing structural support and scaffolding during new bone formation or bone development, other functions of the bone matrix are as follows:
- Serves as a reservoir of minerals, especially calcium and phosphate: Calcium and phosphate are stored as hydroxyapatite crystals in the bone matrix. Hydroxyapatite is converted back into calcium and phosphate ions (via enzymes and acids), especially during bone resorption (removal of old bone tissue by osteoclasts), bone remodeling, acid-base balance, or in the presence of mechanical stress on bones (e.g., weight-bearing exercises).
- Renders bone a degree of flexibility: The bone matrix renders bone a degree of flexibility. So while rigid, the bone also has to be somewhat flexible to make the bone less susceptible to fractures.
- Supporting cell communication: bone matrix holds various proteins, growth factors, and signaling molecules for cell communication and regulation.
Bone Defects and Diseases
Bone defects and diseases refer to conditions affecting the natural bone structure, function, and health of bones. Some examples of bone impairments are as follows:
- Fractures. Injuries in bones, such as breaks in the continuity of a bone may occur due to trauma, falls, or excessive stress on the bone. Fractures may be open or closed depending on whether the bone protrudes through the skin or not.
- Osteoporosis: Metabolic bone diseases, including osteoporosis, affect the bone phenotype, leading to alterations in bone structure and composition. An osteoporosis bone matrix is characterized by a reduced bone mineral density (pertaining to the amount of mineral content in bone) and increased bone turnover (i.e., the process of continuous bone remodeling, involving bone resorption by osteoclasts and bone formation by osteoblasts), resulting in weakened bones and greater fracture risk.
- Osteogenesis Imperfecta: Also known as brittle bone disease, this genetic disorder affects the production of Type I collagen, leading to bones that are weak and prone to fractures even with minimal impact.
- Woven bone: Woven bone, which is a rapidly formed and disorganized type of bone, can be present in bone defects and fracture calluses during the early stages of bone repair.
Treatments and Management
Here are examples of how bone impairments are treated or managed:
- Bone grafts, including autologous bone grafts, are commonly used to treat bone defects and aid in bone repair in cases of non-union or large bone defects.
- Bone tissue engineering involves using biomaterials like demineralized bone matrix and viable bone matrix, combined with cells and growth factors, to promote bone tissue regeneration. Endothelial cells play a crucial role in bone tissue engineering as they contribute to vascularization, which is essential for supplying nutrients to the newly regenerated bone.
- Regular weight-bearing exercises aid in overall bone health and prevent bone-related conditions such as osteoporosis. Mechanical stimuli incite the bone matrix to respond by modifying its structure and composition to meet the demands placed upon it.
NOTE IT!
“Special Bone Matrices of Mammals”
Although mammalian bone is basically made up of the same fundamental organic and inorganic components, some mammals just have these bone matrix features that are distinctively theirs. Here are some examples:
- Dense Cortical Bone in Marine Mammals: Marine mammals, such as whales, dolphins, and seals, have a specialized bone matrix that aids in their buoyancy in water. They are relatively less dense than those of land mammals, helping them remain buoyant while diving and swimming.
- Cancellous Bone Structure in Climbers and Jumpers: Mammals that are skilled climbers or jumpers like primates and squirrels often have a high proportion of cancellous (spongy) bone in their long bones. Cancellous bone is lighter than cortical bone and offers greater flexibility and shock absorption, enabling them in their agility and acrobatic movements.
- Pneumatization of Bones: Pneumatic bones are bones that are hollow from the inside. Some mammalian bones (e.g., the human skull) are pneumatized, meaning they contain air-filled spaces that reduce bone weight. Pneumatic bones of birds such as the humerus, femur, vertebrae, and cranial bones help birds reduce overall body weight making flight more energy-efficient.
Take the Bone Matrix – Biology Quiz!
References
- Henrikson, R., Kaye, G. & Mazurkiewicz, J. (1997). Histology. Baltimore: Williams & Wilkins. p.129
- Eroschenko, V. & Fiore, M. (2008). DiFiore’s atlas of histology with functional correlations. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p.80
- Lin, X., Patil, S., Gao, Y., & Qian, A. (2020). The Bone Extracellular Matrix in Bone Formation and Regeneration. 11. https://doi.org/10.3389/fphar.2020.00757
©BiologyOnline.com. Content provided and moderated by Biology Online Editors.