Chondroblast
n., plural: chondroblasts
[ˈkɒndrəʊˌblæst]
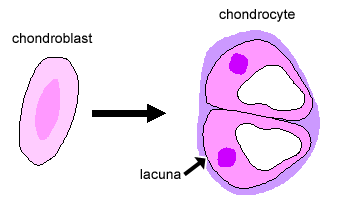
Definition: A cell that may grow into a chondrocyte
Table of Contents
There are two forms of cells in cartilage: chondroblasts and chondrocytes. The chondroblasts are cells that secrete the major component of the cartilage, i.e. the extracellular matrix (ECM). Some chondroblasts may be entrapped inside the ECM that they secrete. When that happens they become less active in producing ECM and turn into chondrocytes that function mainly in the diffusion of nutrients and other substances and the repair of the matrix.
What are chondroblasts?
Chondroblasts are young, immature cartilage cells that eventually form chondrocytes via a process of chondrogenesis. Chondroblasts are also known as subchondral cortico-spongious progenitors or perichondrial cells.
The process of cartilage formation is known as chondrogenesis. Cartilage is a specialized connective tissue that is flexible, strong, and semi-rigid. It consists of chondrocytes and extracellular matrix (ECM). Chondroblasts originate from the mesenchymal stem cell.

Interestingly, chondrocytes are the chondroblasts cells embedded in the ECM, which is made up of proteoglycan and collagen fibers. Hence, chondroblasts and chondrocytes are the different cells you will see in the cartilage.
Now, let’s understand the difference between the chondroblast and chondrocytes.
Table 1: Differences between chondroblasts and chondrocytes | |
|---|---|
| Chondroblast | Chondrocytes |
| Chondroblasts are the developmental cartilage cells that are involved in the development of the cartilage tissue | Chondrocytes are mature cartilage cells that function to maintain the cartilage structure. |
| These cells actively produce the component of the ECM. | These cells secrete ECM and are embedded in it. |
| These cells originate from a type of mesenchymal progenitor cells. | These cells originate from the chondroblasts. |
| Immature cartilaginous cells | Mature cartilaginous cells |
| Appositional growth of the cartilage by chondroblasts | Interstitial growth of the cartilage by chondrocytes |
| Main function is to produce chondrocytes and components of the ECM | Primarily, to maintain the structure of the cartilage and ECM |
Chondrocytes and chondroblast help to maintain homeostasis in cartilage. When chondrocytes in existing cartilage get damaged, an interesting process occurs. It gets converted to chondroblast cells. Damaged chondrocytes in cartilage would result in a loss in the cartilage tissue. The conversion of chondrocytes to chondroblast helps in restoring the cartilage tissue by secretion of the ECM. However, the lack of blood vessels in the cartilage tissue slows down the cartilage regeneration process.
Structure
Chondroblasts are located within the perichondrium. The perichondrium is the vascularized peripheral connective tissue. The function of the perichondrium is to protect the cartilage. The outer layer of the perichondrium is fibrous while the inner layer is chondrogenic, which gives rise to chondroblast cells.
The production of chondroblast cells from the chondrogenic layer is influenced by hormones like growth hormones, thyroid hormones, and glycosaminoglycans.
Chondroblast cells result in appositional cartilage growth, i.e., an increase in the diameter of the cartilage. Chondroblasts cells are irregular in shape and do not poses blood and lymphatic supply.
Interestingly, perichondrium is not present in the articular cartilage.

Matrix formation and composition
The chondroid matrix (i.e., the ground substance of the cartilage) is made up of collagen, proteoglycans, glycoproteins, hyaluronic acid, water, and macromolecules that are secreted by the chondroblasts. These components provide characteristic strength, structure, and tensile strength to the cartilage.
ECM is a gelatinous structure that can absorb water like a sponge. ECM posses unique mechano-physical properties, namely:
- Mechanical property, i.e., strength, structure, and tensile strength of the cartilage, is due to the presence of collagen in it
- Physical property, i.e., swelling and elasticity of the cartilage, is due to the presence of the proteoglycans, primarily aggrecan. The presence of such components makes cartilage a highly hydrous structure.
Chondronectin binds glycosaminoglycans & collagen fibers, which, in turn, provides adherence to chondrocyte and chondroblasts.
Development
The development of cartilage, i.e., chondrogenesis, is an essential physiological function and cartilage. It serves multiple roles at different stages of life. Most importantly, in the embryonic and post-natal phases, cartilages serve as the template for bone development.
Mesenchymal cell condensation and chondroprogenitor cell differentiation initiate chondrogenesis. This triggers the differentiation of chondroblasts.
Chondroblast differentiation is characterized by the conversion of a fibroblast-like cell shape to a spherical cell formation along with the secretion of ECM components chiefly of type-2 collagen (Col2) and aggrecan. Multiple signaling pathways critically influence this onset of chondroblast differentiation. The most prominent signaling pathway that affects chondroblast differentiation is the retinoic acid signaling pathway. Retinoic acid is the primary metabolite of vitamin A. Therefore, a well-balanced level of retinol or retinoic acid is required at the time of chondroblast differentiation. Conversely, a high-level or a low-level of retinoic acid can negatively affect chondrogenic differentiation.
The other transcription factors that affect the chondroblast differentiation include Sox9, Sox5, and Sox6 which encode Sry-related transcription factors. Amongst these, Sox9 is considered to be a master switch for the induction of chondroblast differentiation. The action of Sox9 is under the influence of retinoid.
Inhibition of receptor-mediated retinoid signaling results in the initiation or the induction of the differentiation of chondroblast cells. Thus, levels of retinoid during the differentiation phase of chondroblast are critical. Any imbalance in the vitamin or retinoid levels during pregnancy may lead to skeletal malformation. For this reason, maintenance of Vitamin A levels in pregnant women is critical to avoid any skeletal malfunctioning.
Malfunctioning chondroblasts can result in tumors or cancers—for example, unregulated cell division and growth in chondroblast results in chondrosarcoma or chondroblastomas. Chondrosarcomas is the malignant tumor formation that forms due to malfunctioning chondroblasts. This is one of the most common types of cancer that accounts for almost 30% of bone cancers. On the other hand, chondroblastomas are benign tumors. These tumors are formed at the endochondral ossification sites, i.e., sites where bone replaces the cartilage. Thighbone (femur), shinbone (tibia), or humerus (the upper arm) are some of the most common sites for chondroblastoma formation. Similarly, malfunctioning hypertrophic chondrocytes can result in osteoarthritis and bone growth.
Chondroblasts Function
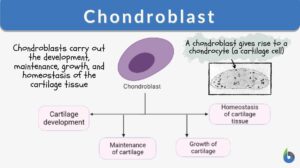
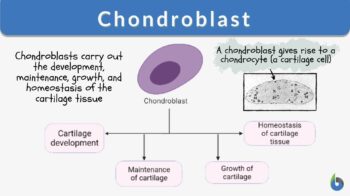
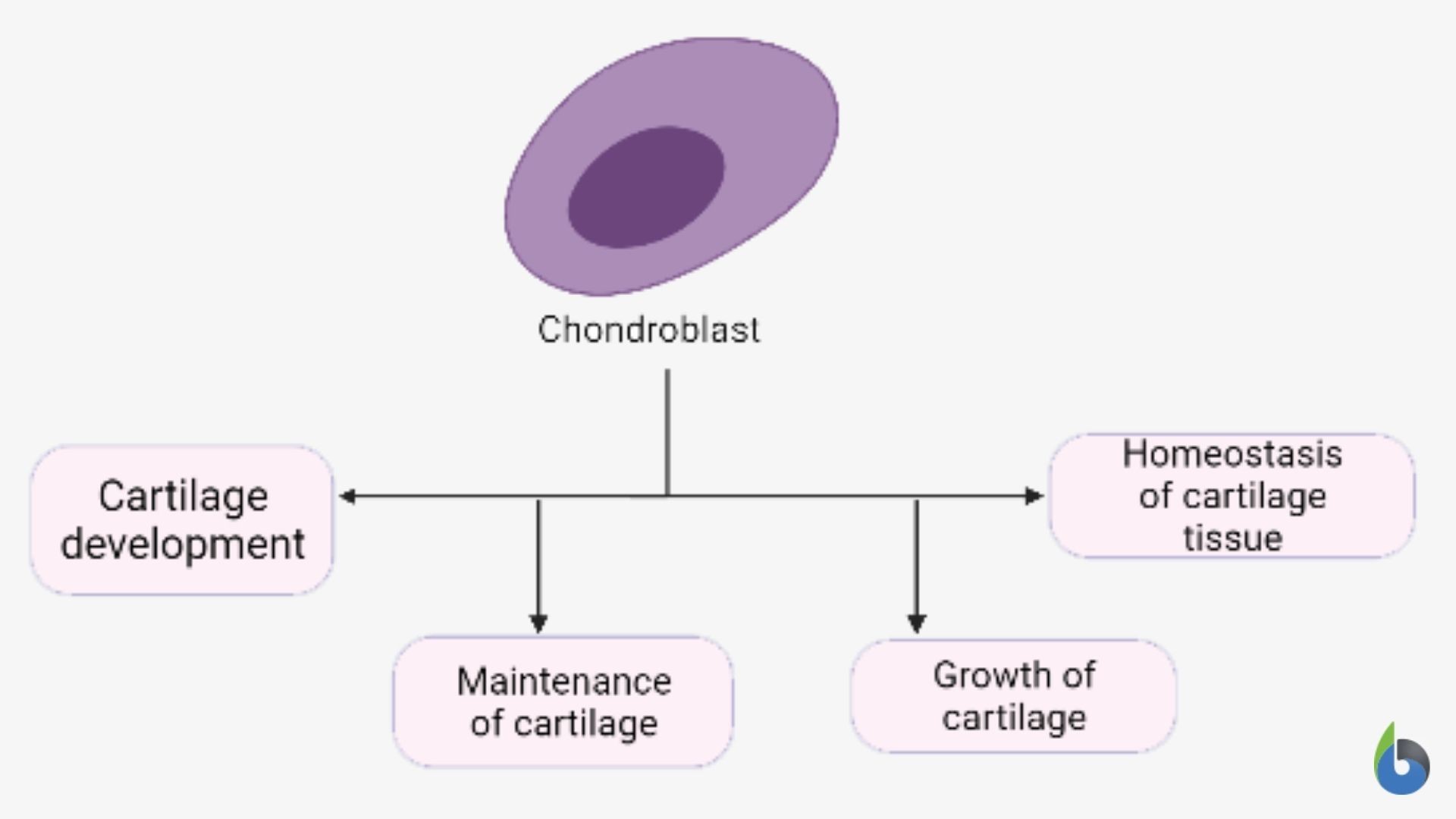
Now, let us understand what chondroblasts do. Chondroblast cells function to carry out the development, maintenance, growth, and homeostasis of the cartilage tissue. Their functions are as follows:
- Development of cartilage: The primary function of the chondroblast is the development of the cartilage. Chondroblasts found in the inner layer of the perichondrium are involved in the development of cartilage. Chondroblast cells transit or mature to form chondrocytes, which form the cellular structure of the cartilage tissue.
- Maintenance of cartilage: Chondroblast also helps maintain the structure and strength of the cartilage tissue by producing components of the ECM.
- Growth of cartilage: Chondroblast cells carry out appositional growth of the cartilage, i.e., thickening of cartilage tissue. The supplementation of the ECM to the peripheral cartilage results in the lateral growth or thickening of the cartilage.
- Homeostasis of cartilage: Chondroblast cells in combination with the chondrocyte cells maintain the homeostasis of the cartilage tissue. There is a conversion of chondrocytes to chondroblasts when cartilage tissue gets damaged. These converted chondrocytes cells then get involved in the regeneration of the lost cartilage tissue, thus maintaining the homeostasis of the cartilage.
- Chondroblast cells are also involved in the Endochondral ossification that leads to bone formation. Briefly, endochondral ossification is the process wherein a bone systematically replaces growing cartilage in order to develop the skeletal system. Unchecked or unrestricted growth of the chondroblasts can result in tumors (chondroblastoma, a benign tumour) and cancers (chondrosarcoma, malignant tumour).
Try to answer the quiz below to check what you have learned so far about chondroblasts.
References
- Aubin, J. E., Liu, F., Malaval, L., & Gupta, A. K. (1995). Osteoblast and chondroblast differentiation. Bone, 17(2 Suppl), 77S–83S. https://doi.org/10.1016/8756-3282(95)00183-e
- Gentili, C., & Cancedda, R. (2009). Cartilage and bone extracellular matrix. Current pharmaceutical design, 15(12), 1334–1348. https://doi.org/10.2174/138161209787846739
- Hoffman, L. M., Weston, A. D., & Underhill, T. M. (2003). Molecular mechanisms regulating chondroblast differentiation. The Journal of bone and joint surgery. American volume, 85-A Suppl 2, 124–132. https://doi.org/10.2106/00004623-200300002-00017
- Shum, L., & Nuckolls, G. (2002). The life cycle of chondrocytes in the developing skeleton. Arthritis research, 4(2), 94–106. https://doi.org/10.1186/ar396
©BiologyOnline.com. Content provided and moderated by Biology Online Editors.