Fibrocartilage
n., plural: fibrocartilages
[faɪbɹəʊˈkɑɹ.təl.ɪd͡ʒ]
Definition: a tough form of cartilage with a matrix of dense bundles of fibers
Table of Contents
What Is Fibrocartilage?
Fibrocartilage is the strongest transitional connective tissue made up of collagen fibers and chondrocytes. Fibrocartilage is a cross between hyaline cartilage and dense connective tissue. The presence of collagen fibers makes this tissue resilient while cartilage tissue provides elasticity. It is found at the site that undergoes repetitive stress like entheses and intervertebral discs. Let’s take a further look at the definition of fibrocartilage.
As the name itself suggests, the term “fibrocartilage” is a combination of the words “fibre” (fiber) and “cartilage” = “fibrous cartilage”.
Fibrocartilage is a transitional connective tissue that is devoid of perichondrium and has structural and functional similarities to both cartilage and dense fibrous connective tissue. The fibrous tissue provides toughness and flexibility to the tissue while the cartilage tissue provides elasticity to the tissue. Fibrocartilage is also referred to as white fibrocartilage.
In biology, the definition of fibrocartilage is as follows: Fibrocartilage is the transitional connective tissue that is present between hyaline cartilage and ligament/tendon. Structurally, the matrix of fibrocartilage is predominantly collagen fibers bundles that are arranged in a parallel fashion for several layers.
In comparison to the other two types of cartilage (i.e., hyaline cartilage and elastic cartilage), fibrocartilage is the strongest and least flexible cartilage. Fibrocartilage provides structural support in the musculoskeletal system.
Fibrocartilage is a dynamic tissue that is found in human wherein entheses is subjected to high mechanical stress and compressional force. Entheses is the site wherein tendon, ligament, capsule, or fascia is inserted into the bone.
Watch this vid about fibrocartilage:
Biology definition:
Fibrocartilage is a type of cartilage that has a fibrous matrix and approaching fibrous connective tissue. The cartilage is a connective tissue characterized by having an extracellular matrix that is abundant in chondroitin sulfate and chondrocytes as the cellular component.
Overview:
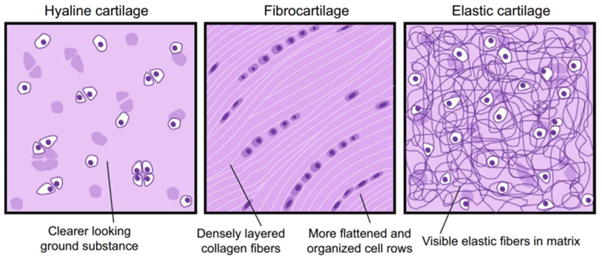
The cartilage has three main types: (1) elastic cartilage, (2) hyaline cartilage, and (3) fibrocartilage. They differ mainly from the fibers that are present. Fibrocartilage is a type of cartilage that has thick layers of larger collagen fibers in the extracellular matrix. This feature enables the fibrocartilage to be fibrous and rough in appearance relative to other types of cartilage. It is the only type of cartilage that has type I collagen apart from the type II collagen normally present in cartilage. The collagen fibers orient themselves in the direction where there is functional stress. Fibrocartilage is found in the pubis symphysis, the annulus fibrosus of intervertebral discs, the menisci, and the temporomandibular joint.
See also: cartilage, connective tissue
Structure
Fibrocartilage is a white, dense tissue with dense fibrous tissue and cartilage tissue in proportions depending upon the site in the body. Alternating layers of hyaline cartilage matrix layer and thick layers of dense collagen fibers provide resilience and strength to the fibrocartilage.
The dense collage fibers are generally oriented in the direction of stress/force applied to them. The matrix of fibrocartilage characteristically contains Type I collagen in addition to the Type II collagen.
Since the cartilaginous tissue of fibrocartilage is a blend of cartilage and fibrous connective tissue, it contains both chondrocytes and fibroblasts. However, it is difficult to distinguish between the two cells in fibrocartilage.
The structure of fibrocartilage is shown in Figure 1.
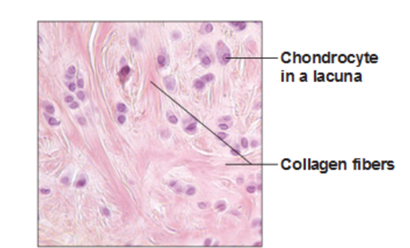
The structural characteristic feature of fibrocartilage includes the following parts:
Cells
The cells present in the matrix of fibrocartilage include both fibrocytes and chondrocytes. These cells are either arranged longitudinally or are irregularly placed in the matrix. Although depending upon their location, the type of cells differs in population For example, the cells in the fibrocartilage of the knee joint menisci are regarded as chondroid tissue as chondroitin sulfate is not found around the cells.
Fibers
All three types of collagen fibers — Type I, II, and III — are found in the fibrocartilage tissue. Depending upon the location, collagen fibers are either irregularly arranged or form a distinct pattern. For example, knee joint menisci have collagen fibers as circumferential hoops while in the attachment zone, collagen fibers are arranged in the long axis of tendons or ligaments. In contrast, in the fibrocartilaginous regions around bony pulleys, collagen fibers distinctly form a basket weave pattern.
Extracellular matrix
Matrix or ground substance of fibrocartilage tissue is amorphous in nature wherein the major constituent is proteoglycans (like chondroitin sulfate). However, the amount of proteoglycan present in the fibrocartilage is more than in the fibrous tissue and less than in the hyaline cartilage.
Blood supply
Fibrocartilage tissue has poor blood supply (avascular) and exhibits a complete lack of blood supply in the knee joint menisci, menisci of the wrist, temporomandibular joints, and tendon/ligament attachment zones.
Note it!
The tensile strength of fibrocartilage is between hyaline cartilage and tendons. The tensile strength of fibrocartilage is ~10 Mpa; the tensile strength of hyaline cartilage is ~4 Mpa. The tensile strength of the tendon is~55 MPa. So, the order of tensile strength of these tissues from highest to lowest is as follows:
Tendon > Fibrocartilage > Hyaline cartilage
Hyaline Cartilage vs. Fibrocartilage
Here, let us also understand the difference between hyaline cartilage and fibrocartilage
Table 1: Hyaline cartilage vs Fibrocartilage | |
|---|---|
| Hyaline cartilage | Fibrocartilage |
| Hyaline cartilage or articular cartilage is the translucent, blue-whitish cartilage that forms a thin layer on the articular surface on the long bones, ribs, nose, and tracheal ring and is considered a precursor to bones | Fibrocartilage is the cartilage that is made up of compact, thick, parallel bundles of collagen fibers and chondrocytes. |
| Made up of only Type II collagen fibers | Has all three types of collagen fibers, Type I, II, and III |
| Less fibrous, thus low in strength as compared to fibrocartilage | Highly fibrous and thus the most resilient and strongest of the cartilage tissue |
| A large number of chondrocytes are present | Few chondrocytes are present |
| Has perichondrium | Lacks perichondrium |
| Facilitate smooth movement of joints | Facilitate attachment of bone to bone and imparts restricted movement of the joints |
| Found in growing bones, nasal septum, tracheal ring, between rib and sternum | Found in joint capsules and ligaments, intervertebral discs |
Data Source: Dr. Amita Joshi of Biology Online
A comparative structure of all three types of cartilage: Hyaline cartilage, Fibro-elastic cartilage, and Elastic cartilage is represented in Figure 2.
Types of Fibrocartilages
There are four types of fibrocartilages
Intra-articular fibrocartilage
The intra-articular fibrocartilage is found wherein extension and flexion occur without gliding and such fibrocartilage act as a thrust pad. This fibrocartilage helps to provide the stability to joints.
Example: menisci
Note it!
Menisci are the crescent-shaped fibrocartilagenous pads present in the knee that act as a shock absorber, stabilizing the knee and providing lubrication to the knee joint
Connecting fibrocartilage
It is found where fibrocartilage connective tissue functions as a cushion to spread the pressure across the joint. This cartilage is found in joints having limited motion.
Example: intervertebral disks
Stratiform fibrocartilage
The stratiform fibrocartilage is found over the surface of the bone for tendons to glide. This cartilage reduces the friction between tendons and bones.
Examples: tendons of the tibialis posterior and peroneus longus
Circumferential fibrocartilage
The circumferential fibrocartilage is ring-shaped that provides protection to the soft tissues of the joint margins and improves the fit of bones in joints.
Examples: acetabular labrum and glenoid
Locations of Fibrocartilage in the Human Body
In the human body, fibrocartilage is found wherein repetitive stress or compressional force is likely to occur. Some of the parts wherein fibrocartilage is found are as follows:
- Pubic symphysis
- Joint menisci like the knee joint menisci
- Temporal mandibular joint
- Annulus fibrosus of intervertebral discs
- The glenoid labrum of the shoulder joint
- The acetabular labrum of the hip joint
- Entheses or ligament/tendon joints with bone
- Metacarpophalangeal joint of the hand
- The proximal interphalangeal joint of the hand
- Cuboid/retinaculum of foot
- Plantar calcaneonavicular ligament of foot
Functions
Fibrocartilage is the strongest cartilage tissue that primarily functions to:
- Act as a cushion by providing the required resilience to the joints to bear the compressive forces
- Release the stress concentration uniformly at the joints
- As the supporting structure of tendons and ligaments joining the bone
Repair
Fibrocartilage tissue has the capability to repair itself. Repairing is initiated by the chondrocytes present in the fibrocartilage tissue.
Fibrocartilage is also involved in the repair of articular bones and cartilage. In other tissues, such as hyaline tissue, healing of any injury or lesion cause the release of growth factors (like, bone morphogenetic protein, transforming growth factor, and fibroblast growth factor) at the site of injury resulting in the formation of scar tissue (fibrocartilaginous tissue). Thus, the elastic hyaline tissue is replaced by tough, fibrous, and less elastic fibrocartilage tissue, which may lead to dysfunctioning tissue.
Clinical Significance
Most of the disorders related to fibrocartilage are due to traumatic body joint injury and very few pathological disorders associated with fibrocartilages are known. Some of the known injuries related to fibrocartilage of joints are mentioned below.
Bankart and Hill-Sachs lesions
Bankart and Hill-Sachs lesions are damage or injury to the humeral head and glenoid labrum due to anterior shoulder dislocations. Abrupt dislocation of the anterior humeral head can prompt intact rotator cuff muscles and ligaments to cause retraction of the proximal humerus.
This results in the posterolateral aspect of the head of the humerus forcefully affecting the anteroinferior part of the glenoid labrum. These two injuries can happen simultaneously and such patients may be at higher risk of recurrent dislocation.
Posterior shoulder dislocation results in reverse Bankart and reverse Hill-Sachs lesions.
Acetabular labral tears
The acetabular labrum is incomplete circumferential fibrocartilage. Injury/damage/defect may result in the disorder of the acetabular labrum. Trauma or hypermobility or laxity in the acetabulofemoral articulation or impingement of femoroacetabular may result in acetabular labral tears. Age-related dysplastic changes or degeneration of joints may also cause acetabular labral tears.
Intervertebral disc degeneration and herniation
The characteristic feature of herniation and intervertebral discs or intervertebral disk degeneration is the loss of proteoglycan and dehydration. As a result, the intervertebral disc becomes more fibrous and is not able to bear and distribute the stress uniformly. Herniation of the intervertebral disc is a serious disorder and can result in radiating pain in the lower limb on standing for a long duration. Any injury or trauma may also precipitate herniation of the intervertebral disc.
Triangular fibrocartilage complex
The combination of several ligaments and fibrocartilage at the distal radio ulnocarpal interface for a structure referred to as the triangular fibrocartilage complex (TFCC). The TFCC functions to stabilize the distal radiocarpal articulation and act as a shock absorber/ cushion for ulnocarpal articulation.
The injury of TFCC can be either Type I (traumatic) or Type II (degenerative). Fall on the outstretched hand (FOOSH) is the most common form of type I injury of TFCC. Distal radial fractures can also damage TFCC.
The injuries/abnormalities to TFCC may be classified as palmer classification.
Table 2: Palmer classification fo TFCC diseases | ||
|---|---|---|
| Disease due to trauma/injury | Degenerative disease | Stage of disease |
| Perforation of TFCC | Wearing of TFCC | Stage A |
| Wear and tear or avulsion of the ulna may result in a distal ulnar fracture | Wearing of TFCC along with chondromalacia of lunate and ulna | Stage B |
| Wear and tear (avulsion) of the distal ulna | Perforation of TFCC along with chondromalacia of lunate and ulna | Stage C |
| Wear and tear (avulsion) of radial | Perforation of TFCC along with chondromalacia of lunate and ulna. This is acompanied by perforation of lunotriquetral ligament | Stage D |
| – | Perforation of TFCC along with chondromalacia of lunate and ulna. Additionally, this condition also has perforation of the lunotriquetral ligament and ulnocarpal arthritis | Stage E |
Data Source: Dr. Amita Joshi of Biology Online
Take the Fibrocartilage – Biology Quiz!
Further Reading
References
- Benjamin, M., & Evans, E. J. (1990). Fibrocartilage. Journal of anatomy, 171, 1–15.
- Benjamin, M., & Ralphs, J. R. (1998). Fibrocartilage in tendons and ligaments–an adaptation to compressive load. Journal of anatomy, 193 (Pt 4)(Pt 4), 481–494. https://doi.org/10.1046/j.1469-7580.1998.19340481.x
- Benjamin, M., Qin, S., & Ralphs, J. R. (1995). Fibrocartilage associated with human tendons and their pulleys. Journal of anatomy, 187 ( Pt 3)(Pt 3), 625–633.
- Buchanan J. L. (2022). Types of Fibrocartilage. Clinics in podiatric medicine and surgery, 39(3), 357–361. https://doi.org/10.1016/j.cpm.2022.02.001
- Clark, R. (2005). Anatomy and physiology : understanding the human body. Sudbury, Mass: Jones and Bartlett Publishers. p. 67.
- Mow, V. & Huiskes, R. (2005). Basic orthopaedic biomechanics & mechano-biology. Philadelphia: Lippincott Williams & Wilkins. pp. 182-183.
- Eroschenko, V. & Fiore, M. (2008). DiFiore’s atlas of histology with functional correlations. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 71-72.
©BiologyOnline.com. Content provided and moderated by Biology Online Editors.