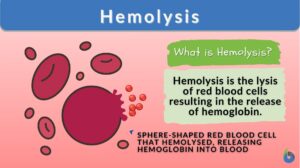
Hemolysis
n., plural: hemolyses
[hɪˈmɒl ə sɪs]
Definition: lysis of the red blood cell, releasing hemoglobin
Table of Contents
The breakdown or catabolism of red blood cells or erythrocytes that result in the expulsion of hemoglobin and other cytoplasmic content in the surrounding fluid or blood circulation is referred to as hemolysis. When the rate of hemolysis is higher than the rate of production of new red blood cells in the body, it results in hemolytic anemia.
What Is Hemolysis?
Hemolysis = Heme (~blood) + Lysis (~breakdown). Hence, the literal meaning of the word, hemolysis or haemolysis is the breakdown of red blood cells or heme i.e., red blood cells (RBCs). In biology, the breakdown of erythrocytes or RBCs is defined as hemolysis, as a result of which the content of RBCs i.e., cytoplasm containing hemoglobin (hemoglobin is the pigment in RBC that carry oxygen) is released into the fluid surrounding it i.e., blood (Figure 1).

RBCs or erythrocytes form the essential component of the blood and these cells are flattened disc-shaped cells that contain hemoglobin in them. Hemoglobin is the iron-containing metalloprotein that binds with oxygen and thus facilitating the transportation of oxygen throughout the body. The RBCs are produced in the bone marrow and have a normal life span of an RBC is 120 days hence, in the natural course the erythrocyte turnover occurs at the end of 120 days to replace the old ones. This process of extravascular hemolysis occurs in the spleen. Hemolysis occurring in the spleen drives erythrocyte turnover. Thus, red blood cell destruction is a natural process that ensures that old RBCs are replaced with new ones and that the iron present in the hemoglobin is recycled for its further usage.
Apart from the natural life cycle of hemoglobin, the destruction of red blood can occur due to a variety of reasons, such as hemolysis due to toxins released by pathogenic microbes, intense exercise, and certain drugs. Such external factors may result in the breakdown of RBCs at a faster rate as compared to their regeneration. This may result in an RBC deficient condition in the body.
Certain internal factors like an autoimmune disorder, hereditary disorders like sickle cell diseases and thalassemia, and abnormal RBCs, may also result in the lysis of RBCs at a faster rate.
The deficiency of RBCs due to excessive hemolysis leads to the condition of hemolytic anemia. To diagnose the condition of hemolytic anemias, free hemoglobin level in plasma or serum is estimated. The normal serum /plasma level of free hemoglobin is 0.02 to 0.05 g/L, however, when the serum /plasma level of hemoglobin increases to 0.3 – 0.6 g/L, it is indicative of a hemolytic condition.
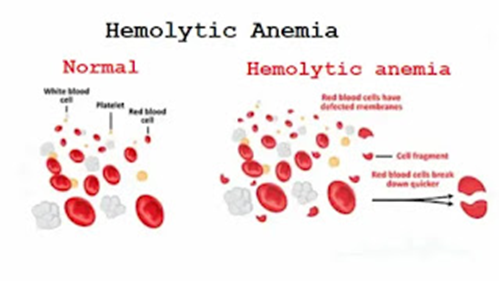
Complete blood count and hematocrit levels are usually measured for diagnosing RBCs level in the blood, i.e., red blood cell count. Thus, hemolysis is an essential controlling mechanism of the body to remove the old and damaged RBCs and replace them with the new RBCs. However, when there is a premature removal of RBCs that exceeds the replacement rate, it results in a hemoglobin-deficient condition known as hemolytic anemia (Figure 2). If uncontrolled, severe hemolytic anemia can be fatal.
Hemolysis may be
- Extravascular or Intravascular
- Episodic or Acute or Chronic
- Acquired or Inherited
- Intrinsic or Extrinsic
Etymology
Hemolysis is derived from the Greek word Heme, αἷμα (haîma, “blood”) and Lysis, λύσις (lúsis, “loosening”).
Hemolysis is the breakdown or catabolism of red blood cells or erythrocytes that results in the expulsion of hemoglobin and other cytoplasmic content in the surrounding fluid or blood circulation. Hemolysis has several causes: examples are exposure of erythrocytes to toxins and poisons, bacterial hemolysins, immune reactions like specific complement-fixing antibodies, hypotonicity, alteration of temperature, treatments such as hemodialysis, etc. In microbiology, the hemolytic reactions of certain microorganisms such as Streptococci on blood agar plates can be used to identify or classify them. For instance, Streptococcus pneumoniae forms alpha hemolysis, Streptococcus pyogenes forms beta hemolysis, and Enterococcus faecalis displays gamma hemolysis on blood agar plates.
Variant: haemolysis
Synonyms: hematolysis; erythrolysis; erythrocytolysis
Inside the Body
Let us understand the conditions under which hemolysis can occur inside the body.
Parasitic hemolysis
Parasitic microbes can invade and break the RBCs present in the blood. The malaria parasite is a widely known parasite that attacks the human blood cells causing hemolysis. Apart from malaria, certain worm infections like whipworm infection (Trichuris trichiura), schistosomiasis (Schistosoma mansoni, S. haematobium, and S. japonicum), hookworm infection (Necator americanus and Ancylostoma duodenale) can also result in hemolysis. Other infectious diseases that can result in hemolysis include Human immunodeficiency virus (HIV), Rocky Mountain spotted fever, Carrion’s disease, Babesiosis, and Haemophilus influenza.
HELLP, pre-eclampsia, or eclampsia
HELLP stands for hemolysis, elevated liver enzymes, and low platelet count. It is a complication of the last trimester of pregnancy or seen in newborns immediately after birth. HELLP is often accompanied by pre-eclampsia or eclampsia. Pre-eclampsia is seen as high blood pressure and high protein in the urine, in pregnant women usually after 20 weeks of gestation. Pre-eclampsia can be dangerous and if untreated can lead to hemolysis, liver dysfunction, reduced platelet count, swelling, shortness of breath due to water retention in the lungs, and visual disturbances.
Pre-eclampsia can be fatal to both the fetus and mother or may result in preterm labor. Untreated pre-eclampsia can result in seizures and this condition is known as eclampsia.
Abnormality in placental development can lead to HELLP and estimating the extent of hemolysis is used as the diagnostic test for it. Levels of lactate dehydrogenase and aspartate transaminase are used as diagnostic tests for HELLP.
In HELLP, microangiopathic hemolysis occurs, which means that RBCs fragment when they pass through small blood vessels having fibrin deposits and endothelial damage. The exact cause and mechanism for HELLP are not known.
Hemolytic disease of the newborn
Hemolytic disease of the newborn or HDN is an autoimmune disorder of newborn babies. In HDN, RBCs of the newborn undergo hemolysis at a very fast rate, this is referred to as erythroblastosis fetalis. This usually occurs due to Rh factor incompatibility.
Humans have either of the four blood groups along with the Rh factor — either an individual is Rh+ve (Rh factor positive) or Rh-ve (Rh factor negative). HDN usually occurs in Rh-ve mothers having a fetus with Rh+ve blood. Fetal RBCs crossing the placenta results in the generation of antibodies in the mother, as the mother’s immune system perceives Rh+ve blood as a foreign element. Thus, the mother’s blood is now Rh-sensitized.
HDN usually is not seen in the first pregnancy as Rh sensitization occurs in it. However, during the subsequent pregnancy, antibodies from the mother against the Rh+ve fetus will cross the placenta during pregnancy or delivery to fight with it resulting in erythroblastosis fetalis. Such babies are born with HDN. HDN babies can develop reticulocytosis and anemia.
Hemolytic anemia
Excessive breakdown of RBCs, at a faster rate as compared to their replacement rate results in hemolytic anemia. Excessive catabolism of RBCs results in a reduced level of hemoglobin in the body resulting in a variety of symptoms including fatigue, lethargy, weakness, dizziness, arrhythmias, and shortness of breath. Hemolytic anemia may be intravascular or extravascular or both in the reticuloendothelial system. Patients with hemolytic anemia have enlarged spleen and/or liver.
Patients with hemolytic anemia also exhibit increased levels of lactate dehydrogenase and unconjugated bilirubin along with reduced levels of haptoglobin levels. The treatment approach for hemolytic anemia may include blood transfusions. Accordingly, the measurement of these diagnostic parameters indicates hemolysis. Hemolytic anemia may be:
- Acquired hemolytic anemia. Patients are not born with the hemolytic condition, certain factors induce hemolysis in them. There can be multiple factors that can induce hemolysis, some of them can be
- Drugs like acetaminophen, penicillin, sulfa drugs, and antimalarial drugs can cause hemolysis.
- Autoimmune disorders like rheumatoid arthritis, lupus, ulcerative colitis
- Overactive spleen
- Blood cancer
- Infectious viral/bacterial disease
- A dysfunctional heart valve may result in damaged red blood cells
- Immune Reaction to blood transfusion
- Inherited hemolytic anemia. Parents pass on the hemolytic condition to their offspring. Here, the life span of RBCs is shorter than the normal life span of an RBC. Examples are sickle cell anemia and thalassemia
- Acquired hemolytic anemia. Patients are not born with the hemolytic condition, certain factors induce hemolysis in them. There can be multiple factors that can induce hemolysis, some of them can be
Hemolytic crisis
Excessive catabolism of RBCs within a very short duration of time and the body is not able to replenish them which results in an acute condition known as hemolytic crisis. Catabolized RBCs get accumulated in the blood and can cause kidney damage. The hemolysis of RBCs results in the release of hemoglobin, which combines with nitric oxide (NO). This results in a reduced availability of vascular NO leading to vasoconstriction, endothelial adhesiveness, and eventually thrombosis.
Excessive hemolysis also results in splenic sequestration (i.e., a huge number of RBCs struck in the spleen) that eventually causes hypovolemia leading to shock. Acute hemolysis can eventually lead to a non-functional spleen.
Toxic agent ingestion or poisoning
Consumption of certain metals and poison can cause hemolysis. The oxidative potential of many chemical substances causes hemolysis. These toxic substances include arsenic, lead, copper, stibine, and snake venom. Ingestion of poisonous fungi, Paxillus involutus may result in hemolysis.
Space hemolysis
Astronauts have been found to have increased red blood cell breakdown due to space travel. A study shows that astronauts at International Space Station have persistently high levels of hemoglobin degradation products, serum iron, and carbon monoxide in alveolar air. These astronauts were reported to have elevated hemolysis and reticulocytosis even 6 months after their space stay. Although the exact cause of this is not known, however, microgravity is hypothesized to play a role in it.
Intrinsic causes
Defects in RBCs themselves can cause hemolysis. This may be due to one or more defective genes that may result in dysfunctional RBCs. Such dysfunctional RBCs have a shorter lifespan. A peripheral blood smear can help to identify the dysfunctionality of RBCs. These defects can be:
- Hereditary elliptocytosis and Hereditary spherocytosis, wherein there is defective RBC membrane production
- Congenital dyserythropoietic anemia, thalassemia, and sickle cell anemia, wherein defective hemoglobin is present.
- Pyruvate kinase deficiency and glucose-6-phosphate dehydrogenase deficiency result in defective RBC metabolism
- Marchiafava-Micheli syndrome or Paroxysmal nocturnal hemoglobinuria (PNH) is s fatal, acquired disease wherein induction of the complement system causes intravascular hemolysis.
Extrinsic causes
In this case, RBCs are normal and healthy, however, due to certain external causes, hemolysis or breakdown of RBCs occurs. Herein, premature RBCs get entrapped in the spleen and eventually break down. Several environmental or external factors may contribute to causing hemolysis; these factors include:
- Autoimmune diseases, e.g., lupus, rheumatoid arthritis, Hodgkin lymphoma, leukemia, and paroxysmal cold hemoglobinuria (which is a type of autoimmune hemolytic anemia). Autoimmune hemolytic anemia is a rare autoimmune disorder wherein antibodies are generated that destroy red blood cells. Autoimmune hemolytic anemia can be of two types — cold autoimmune hemolytic anemia (or cold agglutinin disease) and warm autoimmune hemolytic anemia (or warm autoimmune hemolytic anemia)
- Certain disease conditions like infection by Mycoplasma pneumoniae
- A chronic livers disease is known as spur cell hemolytic anemia
- Conditions like portal hypertension lead to an increase in the activity of the spleen
- Poisoning by metals like lead, arsenic
- Footstrike hemolysis is seen in runners wherein hemolysis of foot RBCs at the site of foot impact is seen. Thus, runners may develop hemolytic anemia
- Infectious diseases like malaria and traumatic condition like burns lead to acquired hemolytic anemia
- Prosthetic heart valve recipients exhibit low-grade hemolysis
Intravascular hemolysis
As the name suggests, when hemolysis occurs within the blood vessels, it is referred to as intravascular hemolysis. Here, the damaged RBCs keep circulating in the blood.
Extravascular hemolysis
As the name suggests, when the hemolysis occurs outside the blood vessels i.e., veins, capillaries, and arteries, it is referred to as extravascular hemolysis. The natural course of replacement of RBCs occurs extravascularly in the spleen. The spleen acts as a filter and blood filters out to remove the old and damaged red blood cells which are further removed by the macrophages.
Did you know? Not all animals have “red” blood…
Hemoglobin accounts for the crimson-red color of many animals, including humans. However, there are animals with blood that isn’t red. Crocodile icefish are the only known vertebrates without hemoglobin when they’re adults. Hence, they are also called ‘white-blooded” fish. And instead of hemoglobin, some animals have an alternative oxygen-transporting chemical in their versions of “blood“. Octopuses and horseshoe crabs have hemocyanin pigment, which makes their blood appear blue. New Guinea’s green-blooded skinks, as the name implies, have green blood. That’s because they have a high level of biliverdin (bile pigment) in their blood (much greater than hemoglobin) which makes their blood impart a green color.
Outside the body
In vitro hemolysis can occur during blood collection and its handling or surgery or in a culture media due to the activity of bacteria.
From specimen collection
Improper blood sample collection, extreme temperature exposure, mishandling during transportation, prolonged sample storage, and delay in blood sample processing are some of the common causes of in vitro hemolysis of the collected blood sample. Inappropriate tube mixing, inappropriate blood collection needle size, prolonged tourniquet, usage of incorrect tubes, excessive suction pressure, and difficult blood collection due to fragile blood vessels are some of the phlebotomy-related factors that cause hemolysis of blood samples. Hemolysis can be induced at the point of venipuncture and may continue till sample processing.
A hemolysed sample causes biological and analytical interference resulting inaccurate results of the diagnostic tests. A hemolysed blood sample is one of the primary causes of pre-analytical error (Figure 3).
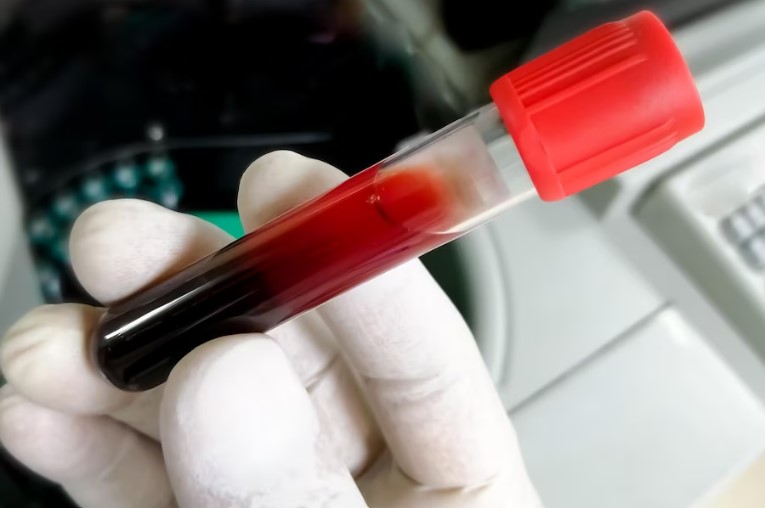
From mechanical blood processing during surgery
Hemolysis can occur during cardiopulmonary bypass surgery wherein a large amount of blood loss is expected, so intraoperative blood salvage machines are used to prevent it. Blood from the patient undergoes centrifugation followed by washing of RBCs with saline and then transported back to the patient’s circulatory system. This is also referred to as extracorporeal circulation. During this whole process of extracorporeal circulation, RBCs undergo mechanical stress during the centrifugation process at a very high speed, resulting in hemolysis.
Mechanical stress faced by RBCs during extracorporeal circulation can result in an immediate or delayed complete breakdown of RBCs. Also, such mechanical stress results in changes in RBCs such as fragile RBCs that agglomerate, reduced deformability, and surface charge. These changes eventually alter the viscosity of the blood.
From bacteria culture
Certain bacterial species like streptococcal species hemolyse the hemoglobin in the agar agar culture media and this also forms the basis of their species identification. Hemolysis is caused by a substance known as hemolysin. Depending upon the streptococcal species, hemolysis can be, α hemolysis (seen in Streptococcus pneumoniae), β hemolysis (seen in Streptococcus dysgalactiae) and ɣ hemolysis (seen in Staphylococcus saprophyticus).
Watch this vid about hemolysis and types:
Nomenclature
Synonyms of hemolysis are hematolysis, erythrolysis, and erythrocytolysis. Hemolysis and hematolysis convey the lysis of hemoglobin whereas eyrthrolysis and erythrocytolysis convey the lysis of erythrocytes.
Complications
Chronic hemolysis can result in multiple organ dysfunction and can lead to a number of complications such as:
- Pulmonary hypertension – As mentioned earlier, the breakdown of RBCs results in the release of hemoglobin, which combines with NO (nitric oxide). This results in reduced levels of NO leading cardiac complications including vasoconstriction, hypertension, and thrombosis.
- Jaundice – Excessive breakdown of RBCs results in the release of heme, which eventually leads to bilirubin buildup. Alongside there is a reduction in plasma proteins, like albumin, hemopexin, and haptoglobin. There is also an increase in levels of stercobilin, a degradation product of heme, in the stool.
- Ischemia
- Kidney dysfunction
- Gall stones
- Thrombosis
- Liver dysfunction
- Iron deficiency
- Arrhythmia, cardiac myopathy, and heart failure
- Dysfunctional spleen
Take the Hemolysis – Biology Quiz!
References
- de Jonge, G., Dos Santos, T. L., Cruz, B. R., Simionatto, M., Bittencourt, J. I. M., Krum, E. A., Moss, M. F., & Borato, D. C. K. (2018). Interference of in vitro hemolysis complete blood count. Journal of clinical laboratory analysis, 32(5), e22396. https://doi.org/10.1002/jcla.22396
· Phillips, J., & Henderson, A. C. (2018). Hemolytic Anemia: Evaluation and Differential Diagnosis. American family physician, 98(6), 354–361.
· Rapido F. (2017). The potential adverse effects of haemolysis. Blood transfusion = Trasfusione del sangue, 15(3), 218–221. https://doi.org/10.2450/2017.0311-16
· Wan Azman, W. N., Omar, J., Koon, T. S., & Tuan Ismail, T. S. (2019). Hemolyzed Specimens: Major Challenge for Identifying and Rejecting Specimens in Clinical Laboratories. Oman medical journal, 34(2), 94–98. https://doi.org/10.5001/omj.2019.19
©BiologyOnline.com. Content provided and moderated by Biology Online Editors.