Leukocyte
n., plural: leukocytes
[ˈluːkə(ʊ)sʌɪt]
Definition: White blood cells
Table of Contents
Leukocytes, also called the white blood cells (WBCs), inhabiting our immune system are the cells that exhibit astonishing adaptability and heterogeneity. From neutrophils to lymphocytes, these cellular defenders relentlessly battle pathogens, orchestrate immune responses and assist in tissue repair. Through intricate signaling and coordinated efforts, leukocytes serve as vigilant sentinels, ensuring our bodies remain resilient in the face of adversity.
If we imagine our bodies to be a bustling metropolis, leukocytes are definitely an incredible team of heroes working tirelessly to protect us from unseen threats. You must be wondering why we say so.
You might be surprised to learn that these heroes aren’t caped crusaders or characters from comic books; they are remarkable biological entities or cells that with their incredible powers defend us against invaders; in the form of bacteria, viruses, viroids, fungi, and other pathogens!
This thriving community of millions of incredible cells known as leukocytes literally patrol our body day in and day out, ever vigilant in their mission to keep us healthy and safe. As they have their specific molecular mechanisms to vanquish invaders and maintain order within your system, the science underlying leukocytes, their structures, types, and functions is mesmerizing!
So, read on and learn about the different aspects of leukocytes with us. ☺
What Are Leukocytes?
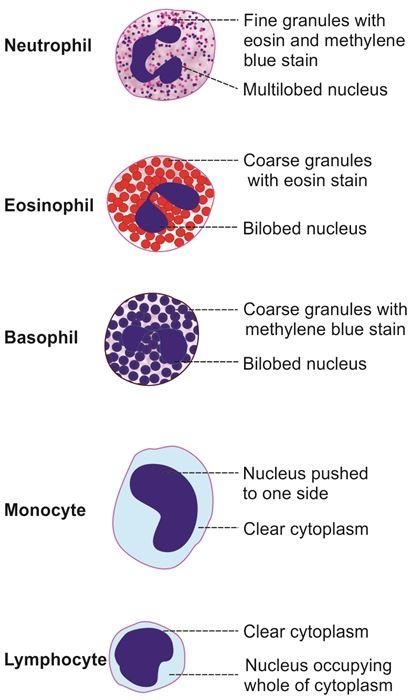
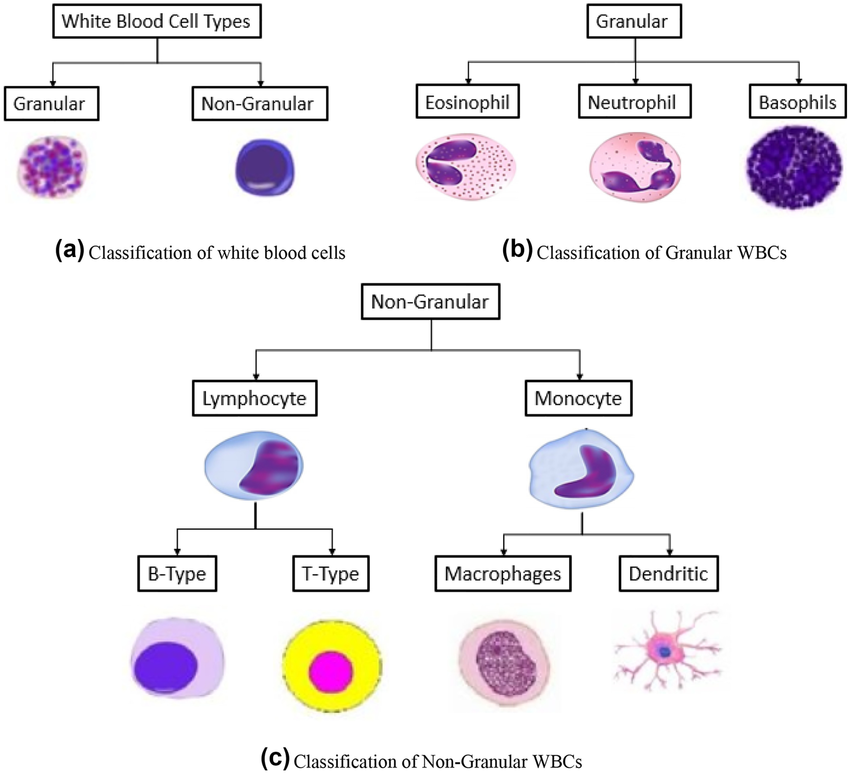
Leukocytes, commonly known as white blood cells (WBCs) are a set of immune cells that come in different shapes and sizes, each with its own unique set of molecular mechanisms to tackle invading pathogens and elements evoking an immune response. They are four main sub-types of white blood or leukocytes; monocytes (plus macrophages), granulocytes (neutrophils, basophils, and eosinophils), lymphocytes (T-cells, B-cells, NK cells), and dendritic cells. Sometimes natural killer cells (NK cells) are considered different from lymphocytes but there are scientific shreds of evidence that NK cells are effector lymphocytes that share their origin with T- and B-cells.
Features common to all leukocytes are:
- They are nucleated blood cells (have a nucleus)
- They lack hemoglobin (unlike red blood cells: RBCs)
- They all are involved in the body’s immune system, thus facilitating the body’s immune response against microorganisms and foreign particles.
- They are also known as white blood cells (WBCs); they separate and form a characteristic thin layer (which is white in color) when whole blood is centrifuged.
- They originated and derived from multipotent stem cells (hematopoietic stem cells/HSCs) in the bone marrow.
- They are found throughout the human body (in the blood and lymphatic tissue system)
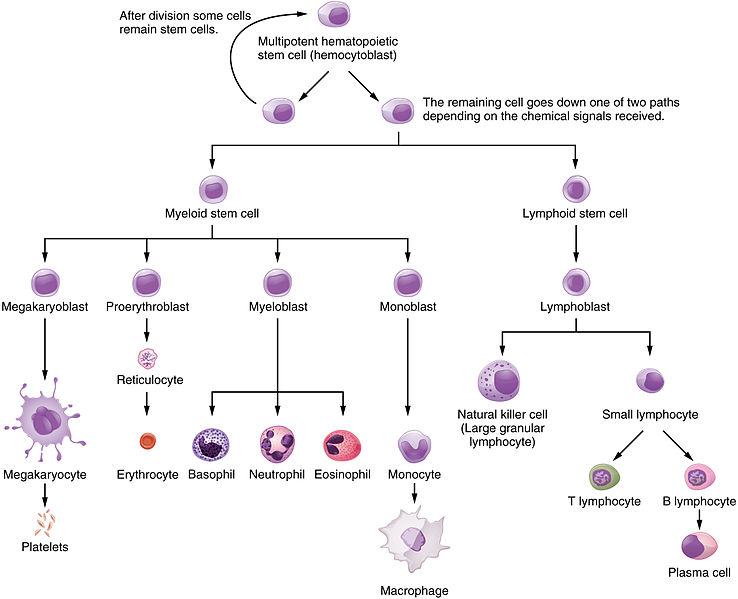
Origin of Different Blood Cells
POINT TO NOTE:
All blood cells originate from a multipotent hematopoietic stem cell (hemocytoblast). The hemocytoblast has two different fates depending on the chemical signal received by the dividing cell:
- Lymphoid Series of Cells divide to give rise to lymphocytes (T-lymphocytes/T-cells, B-lymphocytes/B-cells, natural killer cells (NK cells)
- Myeloid Series of Cells divide to give rise to granulocytes {neutrophils, basophils, and eosinophils}, erythrocytes (RBCs), thrombocytes (platelets), monocytes, and macrophages
- While there is a lot of confusion and despair around dendritic cells’ origin, we would like to clear it up. Dendritic cells are both myeloid and lymphoid in origin. Overall, they can be called “hematopoietic in origin”.
Thus, we can say that overall leukocytes too have a hematopoietic origin. While leukocytes like granulocytes, macrophages, and monocytes have a myeloid origin, on the other hand, NK cells and lymphocytes are lymphoid in origin.
Watch this vid about leukocytes:
Biology definition:
A leukocyte refers to any of the nucleated blood cells that lack hemoglobin, and whose main function involves the body’s immune system, protecting the body against invading microorganisms and foreign particles.
Quick overview:
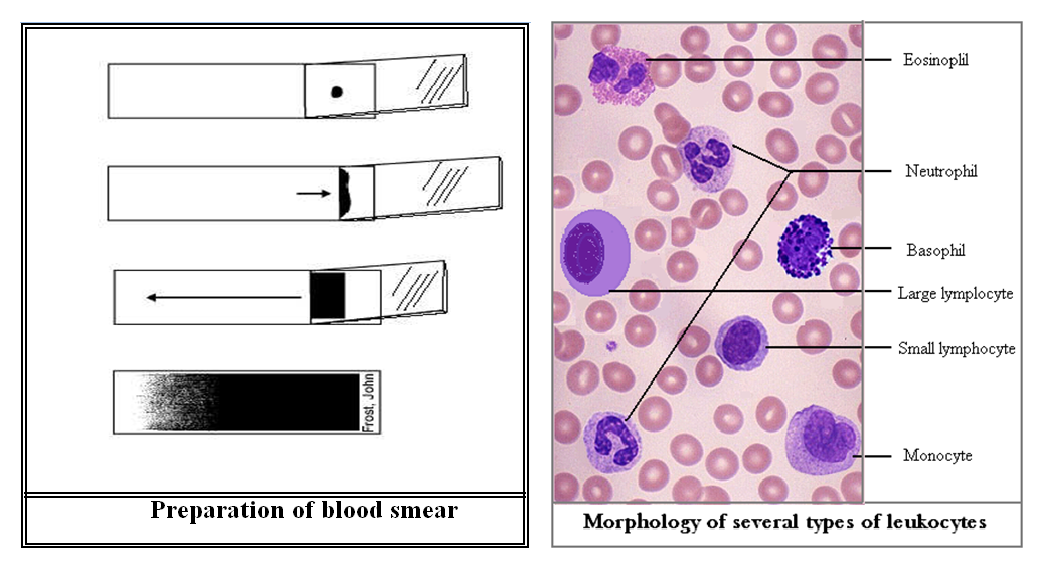
Blood is the circulating fluid in the body of eukaryotic animals. It is primarily composed of plasma and cellular elements (blood cells and platelets). The blood cells with nuclei and lacking in hemoglobin are the white blood cells as opposed to other blood cell types (such as red blood cells). There are different ways to classify leukocytes:
- Based on the presence of granules in the cytoplasm (present or absent, or more precisely, visible on light microscopy or not thus visible): granulocytes (with distinctive cytoplasmic granules, e.g. neutrophils, basophils, eosinophils, and mast cells) vs. agranulocytes (apparently lacking granules, e.g. lymphocytes, monocytes, and macrophages)
- Based on the nuclear lobes: polymorphonuclear (i.e. a nucleus with more than one lobe) leukocytes vs. mononuclear (i.e. a nucleus with only one lobe) leukocytes
- Based on origin: if from lymphoid or myeloid stem cells or both
Synonym: white blood cells (WBC)
Leukocyte Count
The measurement of leukocyte count in both general populations as well as in individuals with specific medical conditions serves as a valuable diagnostic parameter. Its significance in understanding the medical status of patients, especially in clinical settings can’t be overemphasized. In a healthy individual, the leukocyte count typically falls within a specific range with some differences across age groups and laboratories. However, it generally ranges from 4,000-11,000 WBCs per microliter of blood. This count includes different types of leukocytes like neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
Diagnostic Role of Leukocyte Count
The measurement of leukocyte count is an essential diagnostic parameter used by physicians to assess the medical status of patients. It provides valuable insights into the body’s immune response, thus aiding the detection and monitoring of infections, inflammation, and other disease states. By analyzing changes in leukocyte count, healthcare professionals can make informed decisions regarding patient care, treatment strategies, and disease management. Understanding the significance of leukocyte count enables physicians to unravel the intricacies of a patient’s medical condition, thus leading to improved clinical outcomes and better overall healthcare.
Some of the many reasons that physicians look into the leukocyte count of individuals with medical complaints are:
- Infection Detection. Elevations in leukocyte count, particularly neutrophils (a type of white blood cell) often indicate an active infection. The body’s response to infection triggers the release of various signaling molecules that stimulate the production and release of leukocytes from the bone marrow. Monitoring changes in leukocyte count over time can help physicians assess the progress of an infection or the effectiveness of treatment.
Example: Leukocytes are crucial in the body’s defense against urinary tract infections (UTIs) which are often accompanied by foul-smelling urine. Foul-smelling urine can be a result of the metabolic byproducts produced by the bacteria. Elevated leukocyte levels in urine can indicate an infection, as these cells are mobilized to combat invading pathogens like bacteria. Monitoring leukocytes helps diagnose and monitor UTIs, thereby aiding in appropriate treatment and management.
Figure 5: Leukocyte count during UTIs can be instrumental in the detection and development of treatment plans. Image Credit: Brittany N. Bates (Reference-2) - Inflammatory Conditions. Leukocyte count can also serve as an indicator of inflammation within the body. Inflammatory conditions like rheumatoid arthritis or inflammatory bowel disease can lead to increased leukocyte counts. This elevation signifies the body’s ongoing immune response to the underlying inflammatory process. Serial monitoring of leukocyte count aids physicians in evaluating disease activity and determining the effectiveness of anti-inflammatory therapies.

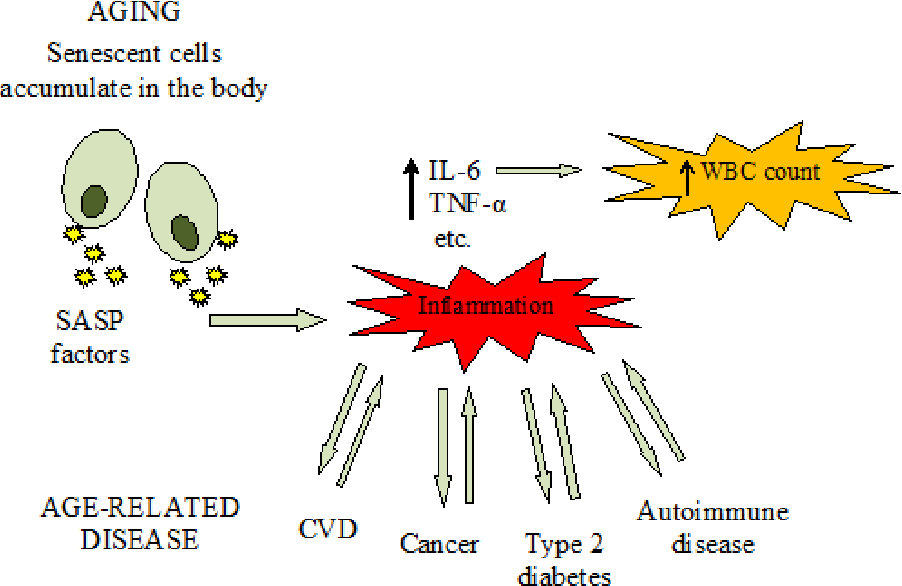
Figure 6: Elevated leukocyte count (WBC count) has been correlated with inflammation. Image Credit: Piotr Paweł Chmielewski (Reference-5) - Leukocyte Count in Disease States. Certain medical conditions can cause specific alterations in leukocyte count.
- Leukocytosis. Leukocytosis refers to an abnormally high leukocyte count often exceeding the upper limit of the reference range. Infections, inflammatory conditions, severe stress, tissue damage, and certain medications may contribute to leukocytosis. Physicians use leukocytosis as an important clue to identify potential underlying causes which helps in diagnostic investigations.NOTE: There is a normal increase in the leukocyte count upon the activation of a healthy individual’s immune system (and this happens frequently). Only occasionally does an abnormal increase in leukocyte count observed which is neoplastic or autoimmune in its nature or origin.
- Leukopenia. Leukopenia denotes a decrease in the number of white blood cells below the lower limit of the reference range. It can result from viral infections, autoimmune disorders, bone marrow disorders, certain medications, or chemotherapy. Monitoring leukocyte count helps physicians evaluate immune function and assess the risks of infection in patients with leukopenia.

Figure 7: Depiction of leukocytosis versus leucopenia condition. Image Credit: Cloud Nine - Cancers. A high white blood cell count can indicate blood cancers, the presence of progenitor cancer cells, or bone marrow disorders. Conditions like leukemia, lymphoma, and myeloproliferative neoplasms (MPNs) can cause abnormal production of white blood cells. Detecting an elevated white blood cell count (or abundant white blood cell count) prompts further diagnostic tests to confirm these conditions. Early identification is crucial for appropriate treatment and improved outcomes.

Figure 8: Conditions related to elevated leukocyte count. Image Credit: AAFP
Location
Deciphering the location of leukocytes has been a curiosity-driven job for most scientists and medical enthusiasts.
- Although some WBCs circulate in the bloodstream, the majority are found outside the circulation residing within tissues.
- These tissue-dwelling leukocytes (WBCs) act as frontline defenders as they directly engage with pathogens at the site of infection.
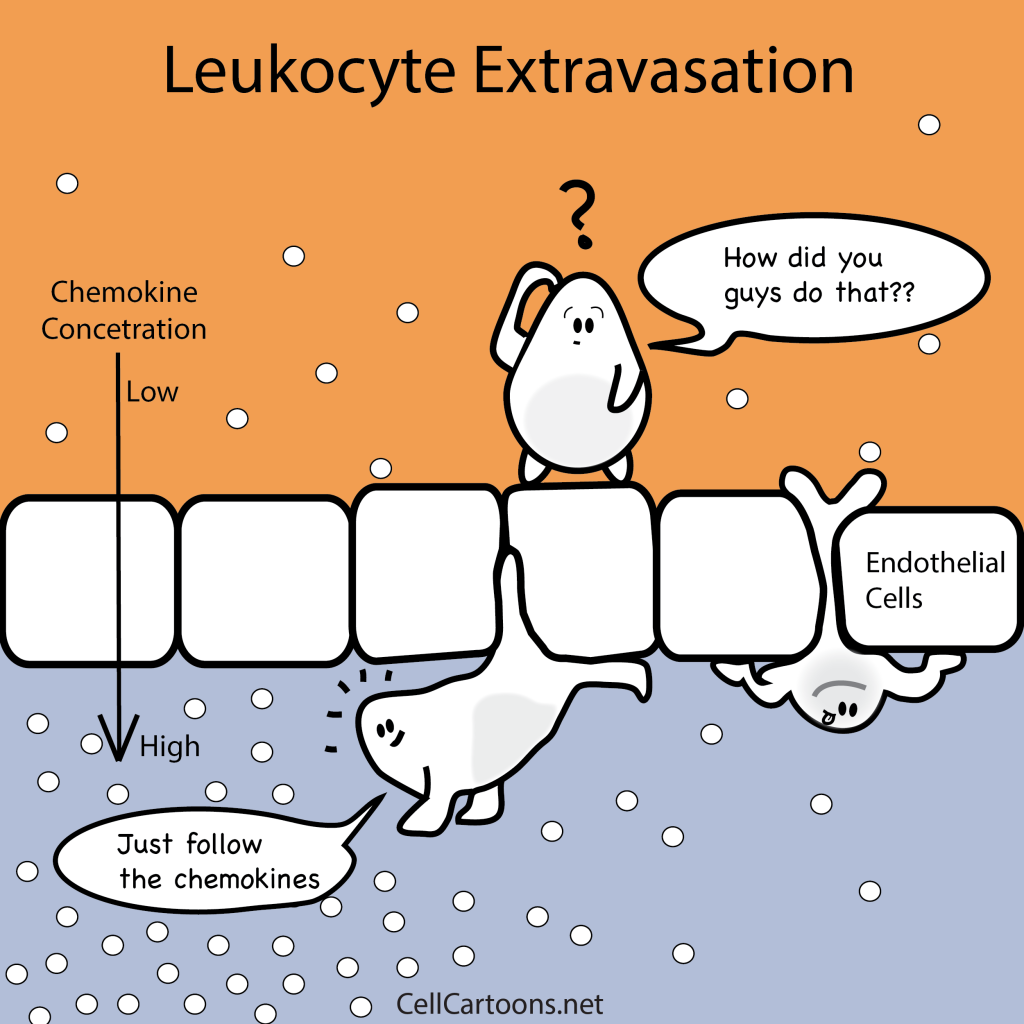
- To reach these tissue locations, leukocytes display remarkable migratory abilities. These are characterized by:
- WBCs undergo a process called diapedesis or leukocyte extravasation, wherein they soften their nuclei and push them to the front edge of their cells.
- This change in shape allows the leukocytes to navigate through blood vessel walls by probing apart the flexible scaffolding made of smaller, threadlike fibers.
- These fibers snap and create temporary openings for the leukocytes to squeeze through.
- Once inside the tissues, the WBCs swiftly locate and eliminate pathogens.
- Despite causing minor disruptions in the blood vessels’ walls, the cells readily repair the breakage as part of their routine cellular maintenance.
- This intricate process of leukocyte migration enables them to combat infections in various tissues throughout the body effectively.
Types
Leukocytes can be classified based on different criteria:
- CRITERIA-1: Presence of Granules
- Granules absent: Agranulocytes (macrophages, monocytes, dendritic cells, and lymphocytes (NK cell, T-cells, and B-cells))
- Granules present: Granulocytes (mast cells, neutrophils, basophils, and eosinophils)
- CRITERIA-2: Origin
- Originating from myeloid stem cells [basophils, neutrophils, eosinophils, mast cells, monocytes, and macrophages]
- Originating from lymphoid stem cells [T cells (including helper T cells, cytotoxic T cells, and memory T cells), B cells (including plasma cells/plasma B cells and memory B cells), and natural killer cells]
- Originating from both lymphoid and myeloid stem cells [dendritic cells]
Fixed Leucocytes
Fixed leukocytes, also referred to as tissue-resident leukocytes, constitute a subset of white blood cells that take up residence within specific tissues of the body. Unlike their circulating counterparts that constantly traverse the bloodstream, fixed leukocytes remain localized within their respective tissues, strategically positioned to fulfill specialized immune functions.
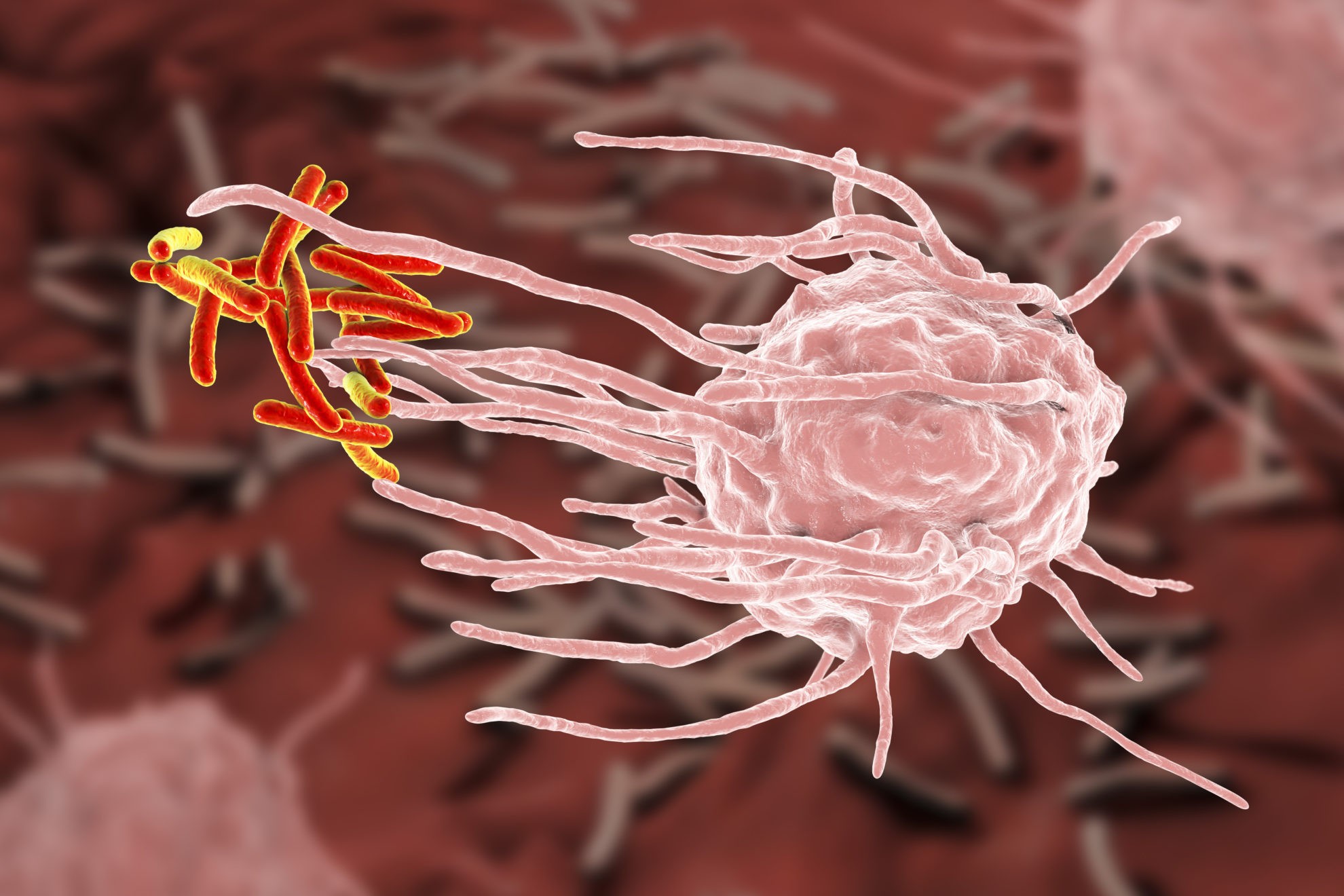
These tissue-resident leukocytes encompass various immune cell types, including macrophages, dendritic cells, and mast cells. Each one of them serves distinct roles and contributes to immune responses within specific tissues.
Examples:
- Macrophages act as phagocytic cells, engulfing and eliminating cellular debris, foreign substances, and pathogens. They play a pivotal role in tissue repair and immune surveillance.
- Dendritic cells function as antigen-presenting cells, capturing antigens and presenting them to other immune cells, thus initiating and coordinating immune responses.
- Mast cells, on the other hand, participate in allergic reactions and release inflammatory mediators.
By residing within tissues, fixed leukocytes actively contribute to tissue homeostasis, immune surveillance, and the initiation of immune responses within their respective tissue microenvironments. This stationary nature enables them to mount swift and targeted immune responses upon encountering pathogens or other immunological challenges in their local tissue surroundings.
Disorders
We have compiled the different types of leukocyte or white blood cell disorders with their description, types/subtypes, causes, symptoms, blood sample diagnostic tests, and treatments in a comprehensive table below.
NOTE: We recommend consulting with healthcare professionals for accurate diagnosis, proper management, and personalized treatment plans for specific leukocyte disorders.
Table 1: A comprehensive compilation of disorders related to leukocytes. | |||
|---|---|---|---|
| Leukocyte Disorder | Description | Causes and Symptoms | Diagnostic Tests & Treatments |
| Leukocytosis | Abnormally high white blood cell count | Causes: Infections, inflammation, medications, stress, underlying medical conditions Symptoms: Fever, fatigue, increased risk of infection, inflammation | Diagnostic Tests: Complete blood count (CBC), differential blood count Treatments: Treat the underlying cause, medication, immune-modulating therapies |
| Leukopenia | Lower than normal white blood cell count | Causes: Viral infections, autoimmune disorders, bone marrow disorders, chemotherapy, radiation therapy Symptoms: Increased risk of infections, weakness, fatigue | Diagnostic Tests: Complete blood count (CBC), differential blood count Treatments: Treat the underlying cause, medication, immune-stimulating therapies |
| Neutropenia | Decreased neutrophil count Types/Subtypes: Congenital neutropenia, cyclic neutropenia, acquired neutropenia | Causes: Inherited (genetic mutations) or acquired (chemotherapy, medications, viral infections, autoimmune disorders, bone marrow disorders) Symptoms: Increased susceptibility to bacterial infections, recurrent infections, mouth sores, fever | Diagnostic Tests: Complete blood count (CBC), differential blood count Treatments: Medications (growth factors, antibiotics), treatment of the underlying cause, preventive measures against infections |
| Eosinophilia | Increased eosinophil count | Causes: Allergic reactions, parasitic infections, autoimmune diseases, certain cancers, drug reactions Symptoms: Allergy symptoms, asthma, skin rashes, gastrointestinal issues | Diagnostic Tests: Complete blood count (CBC), differential blood count, allergy testing Treatments: Treat the underlying cause, medication, allergy management, antiparasitic treatment |
| Basophilia | Increased basophil count | Causes: Allergic reactions, inflammation, certain cancers, hypothyroidism, chronic myeloid leukemia Symptoms: Itching, hives, allergic symptoms, fatigue, joint pain | Diagnostic Tests: Complete blood count (CBC), differential blood count Treatments: Treat underlying cause, medication |
| Monocytosis | Increased monocyte count | Causes: Chronic infections, autoimmune disorders, certain cancers, inflammatory bowel disease Symptoms: Fatigue, fever, night sweats, recurrent infections | Diagnostic Tests: Complete blood count (CBC), differential blood count Treatments: Treat underlying cause, medication |
| Leukemia | Cancer of the bone marrow, abnormal white blood cell production Types/Subtypes: Acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL), chronic myeloid leukemia (CML) | Causes: Genetic mutations, environmental factors Symptoms: Fatigue, weakness, recurrent infections, bleeding, bruising, bone pain | Diagnostic Tests: Complete blood count (CBC), bone marrow biopsy, genetic testing Treatments: Chemotherapy, radiation therapy, targeted therapy, immunotherapy, stem cell transplant |
| Lymphomas | Cancers affecting the lymphatic system Types/Subtypes: Hodgkin lymphoma, non-Hodgkin lymphoma (diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, Burkitt lymphoma, etc.) | Causes: Genetic mutations, environmental factors Symptoms: Enlarged lymph nodes, fever, night sweats, weight loss, fatigue | Diagnostic Tests: Biopsy, imaging tests, blood tests, lymph node biopsy Treatments: Chemotherapy, radiation therapy, targeted therapy, immunotherapy, stem cell transplant |
| Immunodeficiency Disorders | Impaired immune system function Types/Subtypes: Primary immunodeficiency disorders, secondary immunodeficiency disorders | Causes: Genetic mutations (in primary disorders), acquired conditions (in secondary disorders) Symptoms: Frequent or severe infections, poor immune response, recurrent illnesses | Diagnostic Tests: Blood tests (immunoglobulin levels, lymphocyte counts), genetic testing Treatments: Treatment of underlying cause, immunoglobulin replacement therapy, medication, immune-stimulating therapies |
Data Source: Dr. Harpreet Narang of Biology Online
NOTE IT!
How studying “Hematology” can change the entire dynamics?
Hematology is a fascinating field of study dealing with blood and the different types of cells in it. It offers insights into the complexities of the human body and its incredible mechanisms. Here we list a few reasons why blood and its cells are captivating subjects for research that can motivate you to learn it with even more interest.
- A Window into Health and Disease
Blood provides a window into our overall health and well-being. By analyzing the composition and characteristics of blood cells, scientists and medical professionals gain valuable insights into various diseases, disorders, and infections. Abnormalities in blood cell counts, morphology, or functionality can serve as “diagnostic markers and indicators” of underlying health conditions. The study of blood cells helps in the early detection, monitoring, and treatment of diseases like anemia, leukemia, infections, and autoimmune disorders.
- Dynamic and Responsive Nature
Blood is a highly dynamic fluid that constantly responds to changes within the body. The composition and behavior of blood cells can vary depending on factors like exercise, stress, infection, and hormonal fluctuations. This dynamic nature makes blood an intriguing subject of study that allows researchers to conduct “blood investigations and correlate it with different stimuli and conditions” influencing the behavior and functions of blood cells.
- Complex Interactions and Signaling
Blood cells engage in intricate interactions and signaling pathways. White blood cells (WBCs) coordinate complex immune responses to combat infections and diseases. They communicate with each other through chemical messengers, migrate to specific sites, and interact with pathogens or infected cells. Understanding the signaling mechanisms and interactions between blood cells provides “valuable insights into how our immune system works” and can lead to the development of innovative treatments and therapies.
- Blood as a Transport System
Blood serves as a remarkable transport system, delivering oxygen, nutrients, hormones, and waste products throughout the body. Red blood cells, with their unique structure and hemoglobin content, efficiently carry oxygen to tissues and organs. Platelets play a vital role in clotting and prevent excessive bleeding and aid in wound healing. A better understanding of how these transport mechanisms operate can help us in “harnessing the underlying science for medical advancements”.
- Technological Advancements
Advancements in technology have revolutionized the study of blood cells. High-resolution imaging techniques, flow cytometry, genetic analysis, and other sophisticated tools enable researchers to delve deeper into the characteristics and functions of blood cells. These technological advancements have allowed for more precise identification, characterization, and manipulation of blood cells. This has helped in the expansion of our knowledge and opening up “new avenues for therapeutic interventions”.
Take the Leukocyte – Biology Quiz!
References
- Baghel, N., Verma, U., & Nagwanshi, K. K. (2022). WBCs-Net: Type identification of white blood cells using convolutional neural network. Multimedia Tools and Applications, 81(29), 42131-42147.
- Bates, B. N. (2013). Interpretation of urinalysis and urine culture for UTI treatment. US Pharm, 38(11), 65-68.
- Chmielewski, P. P., & Strzelec, B. (2018). Elevated leukocyte count as a harbinger of systemic inflammation, disease progression, and poor prognosis: a review. Folia morphologica, 77(2), 171–178. https://doi.org/10.5603/FM.a2017.0101
- Farhangi, M. A., Keshavarz, S. A., Eshraghian, M., Ostadrahimi, A., & Saboor-Yaraghi, A. A. (2013). White blood cell count in women: relation to inflammatory biomarkers, haematological profiles, visceral adiposity, and other cardiovascular risk factors. Journal of health, population, and nutrition, 31(1), 58–64. https://doi.org/10.3329/jhpn.v31i1.14749
- Chmielewski, P.P. (2018). Leukocyte count, systemic inflammation, and health status in older adults: a narrative review. Anthropological Review, 81, 101 – 81.
©BiologyOnline.com. Content provided and moderated by Biology Online Editors.