Myocardium
n., plural: myocardia
[mī′ō-kär′dē-əm]
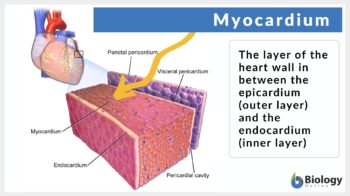
Muscular portion of the heart located in between the epicardium and the endocardium
Source: modified by Maria Victoria Gonzaga, BiologyOnline.org, from the work of Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. Source, CC BY 3.0.
Table of Contents
Myocardium Definition
What is the myocardium of the heart? It is the muscular middle layer of the heart that is sandwiched between the epicardium and endocardium. Sometimes it is referred to as the mass of the heart. The myocardium is made up of two types of cells: cardiac muscle cells (also called heart muscle cells,cardiomyocytes, cardiac myocytes, or cardiac rahbdomyocytes) and fibroblast.
The heart is the central circulatory organ in the human body that circulates the blood throughout the body. The heart is located in a thin fibroelastic, double-layered, fluid-filled sac known as “pericardium”. The two layers of the pericardium are the outer fibrous or parietal pericardium and the inner serous or visceral pericardium.
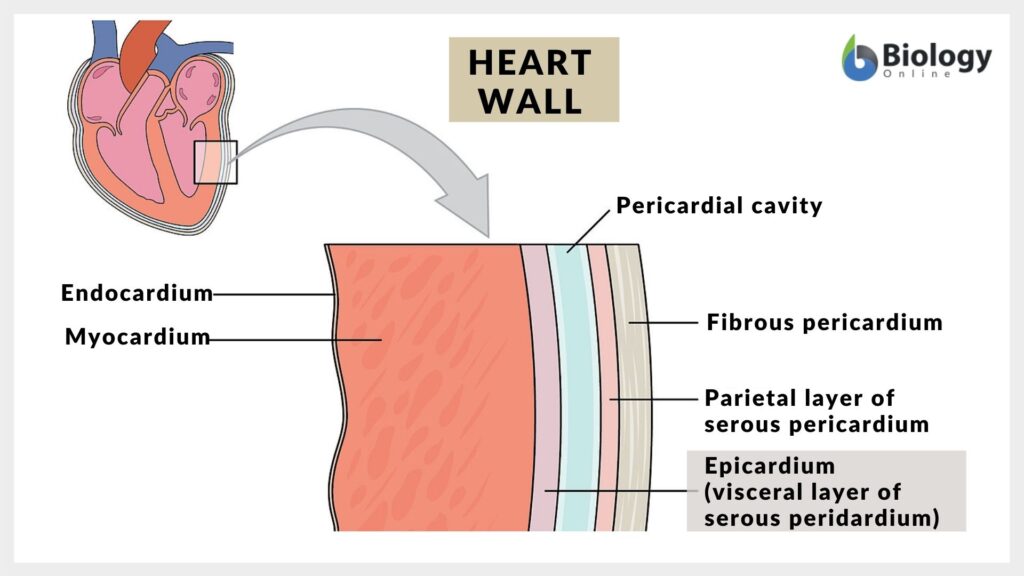
There are three layers in the walls of the heart namely:
- Epicardium: It is the outermost layer of the heart wall. This contains mesothelial cells under which are connective and adipose tissues. This layer also constitutes the visceral layer of the serous pericardium. Below the epicardium coronary arteries and veins, lymphatic vessels, and nerves are present.
- Myocardium: This is the muscle layer of the heart responsible for the pumping action of the heart and occupies 95% of the cardiomyocytes mass and is the thickest layer in the heart wall. The thickness of the myocardial layer is dependant on the pressure which is present in each chamber. So, the question arises out of the four chambers of the heart, which chamber has the thickest myocardium. The myocardial layer is thin in the atrium while the myocardium is thickest in the ventricles specifically in the left ventricle. As a matter of the fact, in adult animals, the left ventricular myocardium is three times thicker than the right ventricular myocardium. This is quite intriguing and instigates the query as to why is the left ventricle thicker than the right ventricle. The walls of the left ventricle of the heart are thicker than the right ventricle since the left ventricle pumps the blood throughout the body and also against the higher pressure in compassion to the right ventricle.
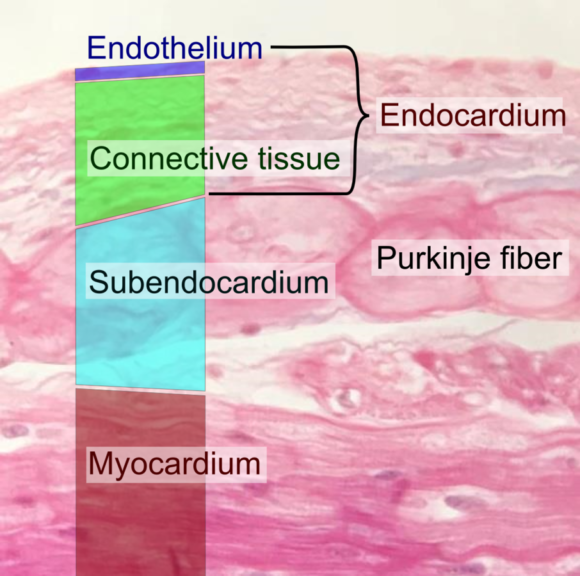
- Endocardium: This is the innermost layer that lines the inner wall of the heart and also lines the heart valves. The endocardium is further subdivided into two layers: (1) an inner endothelial cell layer that lines the heart chamber and (2) the second layer is the subendocardial layer which is a connective tissue layer in continuation with the connective tissue of the myocardial connective tissue layer. The impulse-conduction system of the heart is placed in this subendocardial layer.
Cardiac Muscle Histology
What is cardiac muscle? It is important to understand the definition of cardiac muscles. Basically, cardiac muscles are the involuntary, striated muscles that are made up of cardiac muscle cells or cardiomyocytes.
Cardiac muscles are one of the three types of vertebrate muscles (the other two being, skeletal muscles and smooth muscles). Cardiac muscles share some of the features of both smooth muscles as well as skeletal muscles. Like skeletal muscles, cardiac muscles are striated and can induce strong contractions as well can initiate continuous contractions like smooth muscles. However, cardiac muscles possess certain unique characteristics.
The cardiomyocytes are arranged in a helical or overlapping spiral pattern and are fastened to the fibrous skeleton of the heart. This helical pattern results in a complex 3-dimensional structure network.
Cardiac muscle fibers are elongated cylindrical in shape, approximately 50–100 μm long and 10–25 μm wide. These muscle fibers are made up of distinct quadrangular cells having a centrally located clear oval nucleus. The rectangular-shaped muscle cells are often branched and joined end to end forming a syncytium.
The two cardiac muscle cells meet to form a special junctional complex known as an intercalated disc. These intercalated disks contain three essential components:
- Desmosomes join the intermediate filaments of the cytoskeleton
- Gap junctions that spread of excitation by offering low electrical resistance
- Adhering junction or fascia adherens are the connections with the actin filaments to transmit contraction

Structurally, intercalated disk represents the double membranes formed due to tightly bound cells by desmosomes that are connected by gap junctions. This is required for transferring cell-to-cell electrical impulse conduction. Gap junctions aid in the electrical coupling of the muscle cells, thereby promoting the synchronized beating of the heart muscles.
Cardiac muscle cells are capable of strong, continuous, and rhythmic contractions generated automatically. Though, the autonomic nervous system and hormones can alter the contractility of the heart muscle cells.
Under a microscope, intercalated disks can be seen as faint lines running perpendicular to the long axis of the cardiac muscle fiber. In the adult human, a brown color pigment located at a perinuclear position can be usually seen. This brown color pigment is “lipofuscin“, which is considered as “wear and tear” pigment, is the accumulation of the lipids, phospholipids, and proteins after lipid peroxidation.
Sarcomeres are the functional unit of the cardiac myocyte and contraction. Within each myocyte, the contractile fibers of the sarcomeres are surrounded by transverse discs, known as Z-bands. Each myocyte possesses a number of sarcomeres that are stacked end to end and circumferentially forming a “cable effect” within the cell.
There are two important proteins found in cardiac muscle cells are myosin and actin. The thick filaments are made up of myosin while thin filaments are of actin. These two proteins collectively form the myofibrillar filament that functions to carry out the contractile function in the cardiac muscle tissues.
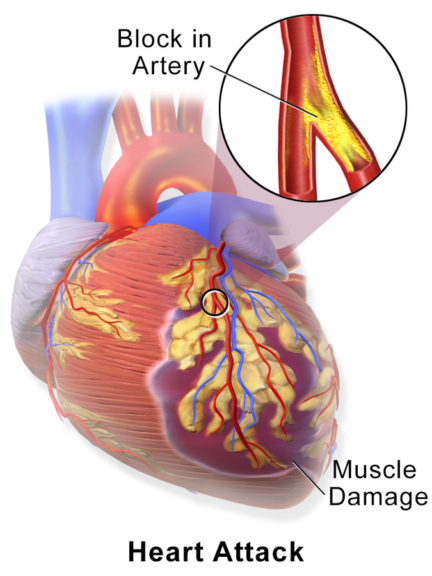
The sarcoplasm (i.e., the cytoplasm of the cardiac myocytes) of the cardiac muscle cells is extremely rich in mitochondria due to the high energy requirement for regular contractions. Oxidative phosphorylation occurs in the cardiac myocytes to meet the energy requirements. Thus, these muscles require an uninterrupted supply of oxygen. The blood is supplied to the myocardium by coronary arteries. Additionally, glycogen granules are present in the myofibrils to support the additional energy requirement.
The myocardium has the largest oxygen requirement and is most critically affected by the reduction in blood flow. Reduction in blood flow i.e. ischemia can be potentially critical for these muscles. Also, cardiac muscles are resistant to fatigue. Essentially, cardiac muscles create their own action potential, i.e. myogenic in nature; however, certain modified muscle cells are specialized to generate the stimulus for the heartbeat and conduct the impulse to different segments of the myocardium system.
These specialized cells form the myocardial conduction system that consists of the sinoatrial node, atrioventricular node, the bundle of His, and Purkinje fibers. 99% of the myocardium is made up of contractile cells while 1% of the cells are part of the myocardial conducting system.
The conducting myocardial cells are specialized muscle cells that function in the same way as neurons. These conducting cells initiate and spread the action potential throughout the heart while the contracting myocardial cells take up this action potential to pump the heart rhythmically and regularly.
Functions of the Myocardium
To understand the circulatory system, it is important to understand what is the function of the myocardium. The primary function of the cardiac muscles is to stimulate contractions and relaxation in the heart. The contraction action results in the pumping of the blood from the ventricles to the whole body while the relaxation action of the cardiac muscles allows the atrium to receive blood. This beating of the heart pumps the blood throughout the body ensuring that each cell and tissue of the body receives the blood supply.
Cardiac muscles are essentially under the control of an autonomous nervous system that releases the timed nervous impulses signaling the heart cells to contract and relax in a rhythmic pattern.
Physiology
So, what actually happens in cardiac muscles when your heart beats? The action potential or nerve impulse stimulates the sarcoplasmic reticulum resulting in the release of calcium ions (Ca2+) into the cytoplasm. The cytoplasmic Ca2+ ions induce the troponin to release tropomyosin. Released Tropomyosin alters its position thereby allowing myosin to attach to actin.
Myosin, then, utilizes the stored ATP molecules and reduce the length of each sarcomere. Contrarily in absence of the impulse, rapid reabsorption of the Ca2+ into the sarcoplasmic reticulum occurs. Thereby, in absence of Ca2+ Troponin re-anchors itself to tropomyosin resulting in the relaxation of the cardiac muscle cells. The cardiac muscle undertakes twitch-type contractions wherein there is a long refractory period followed by brief relaxation periods. The relaxation action is vital for the heart in order to fill the atrium with blood for the next cycle.
All the cardiac muscles work in harmony resulting in the generation of the force on the walls of the chamber of the heart. The sheets of the cardiac muscles are placed in a planar fashion wherein each muscle is perpendicular to each other. This creates the effect that when the heart contracts, it does so in multiple directions. Thus, contraction of the multiple layers of the cardiac muscle fiber results in the shrinkage of the ventricle and atrium from top to bottom as well as from side to side. This produces a strong pumping and twisting force in the ventricles, forcing blood throughout the body.
It is important to note that cardiac muscle undergoes aerobic metabolism, principally utilizing lipids, and carbohydrates.

Myocardium Dysfunction
Myocardial dysfunction can be categorized into two types: primary (due to genetic cause) and secondary myocardial diseases (mostly acquired causes but maybe precipitated due to genetic reasons).
Cardiac myopathy
Cardiomyopathies are diseases that result due to dysfunctional myocardium. Globally, cardiomyopathy is one of the foremost causes of morbidity and mortality. Clinically, cardiomyopathies can be categorized into five categories:
- Dilated cardiomyopathy: Ventricular dilation and exhibit symptoms of congestive heart failure. Arterial hypertension, myocarditis, alcohol abuse, or tachyarrhythmias are some of the main contributing factors to this condition.
- Hypertrophic cardiomyopathy: Hypertrophy of the ventricle, particularly the left ventricle can cause hypertrophic cardiomyopathy. This cardiomyopathy is considered to be genetically transferred via sarcomere.
- Restrictive cardiomyopathy: Scarring and stiffening of the ventricle walls is observed along with impairment of diastolic filling of the heart.
- Arrhythmic cardiomyopathy: Genetically defective desmosomes result in Arrhythmic cardiomyopathy. It is non-ischemic cardiomyopathy generally exhibiting arrhythmias. The majority of the cases reported have a problematic right ventricle though few cases of left ventricles have also been reported.
- Unclassified cardiomyopathy: Cardiomyopathy that does not fall under any of the above cardiomyopathies are classified as Unclassified cardiomyopathy
Myocardial infarction (Heart attack)
Very high quantity and continuous supply of oxygen and energy is the basic requirement of the cardiac tissues. The oxygen supply is transported to the heart via the coronary arteries. However, these arteries are highly disposed to the formation of atheromas, i.e. abnormal deposition of fatty acids, cholesterol, and various cell debris. Incase these atheromas are large, they obstruct or reduce the passage of the blood and oxygen to the cardiac cells thereby leading to the condition known as myocardial infarction or heart attack.
The reduction in the oxygen supply to the cardiac cells is known as myocardial ischemia. The lack of oxygen leads to the death of cardiac tissue. However, under the normal physiological response of the human body, the affected area gets repaired. Though the repairing leads to the formation of fibrous tissue at the site which disturbs the normal propagation and conduction of the excitatory stimuli resulting in abnormal contraction of the heart. These asynchronous contractions result in cardiac arrhythmias i.e., disturbances of cardiac rhythm, e.g. ventricular fibrillation.
Cardiomyopathy
Cardiomyopathy refers to the chronic disease of the heart muscle.
- Ischemic cardiomyopathy: Diffuse coronary atherosclerosis can result in prolonged cardiac ischemia leading to a dilatated type of cardiomyopathy. This may occur after one or multiple episodes of silent myocardial infarction(s).
- Metabolic cardiomyopathy: High levels of blood glucose associated with diabetes mellitus result in ventricular dysfunction resulting in metabolic cardiomyopathy.
- Peripartum cardiomyopathy: Left ventricular systolic dysfunction, within 1-month post-delivery or 5 months post-partum can result in peripartum cardiomyopathy.
- Tachycardia-induced cardiomyopathy: Chronic and persistently high heart rate (>110 beats per minute) as seen in sustained ventricular tachycardia or atrial fibrillation can result in Tachycardia-induced cardiomyopathy. In case, it is not treated it can eventually lead to heart failure.
In case the cardiomyopathy is not treated, it may lead to the following possible conditions:
- Heart failure: Inefficient pumping of the heart results in insufficient blood to meet your body’s needs and can be life-threatening.
- Blood clots: Formation of blood clots can occur and these clots can block the blood supply to the organs including the heart and brain and eventually leading to stroke
- Valve problems: Cardiomyopathy can result in enlargement of the heart thereby resulting in improper closure of the heart valves.
- Cardiac arrest and sudden death: Cardiomyopathy results in cardiac arrhythmias that can result in fainting or, sudden death.
Myocarditis
Inflammation of the myocardium results in myocarditis. This can be attributed to a variety of causes viz., viral infection (infectious myocarditis), toxic substances, drug allergy, bacterial or fungal or parasitic infection, autoimmune disorder. Injury and loss of both cardiomyocytes and cardiac vascular endothelial cells can occur in myocarditis. This results in the infiltration of the white blood cells into the heart muscle wall. This can eventually result in interstitial cardiac fibrosis, wall motion abnormalities, arrhythmias, heart failure, myocardial infarctions, reduced ejection fraction, and sudden cardiac death. Myocarditis can be manifested as chest pain, dyspnea, flu-like manifestations; sometimes it can be asymptomatic as well.
Heart failure
The common end-stage pathway and the manifestation of cardiac dysfunction that may result due to a variety of pathophysiological causes results in Heart failure or congestive heart failure. Heart failure is the inability of the heart to pump an adequate amount of blood throughout the body resulting in congestion, reduced organ perfusion, and functional impairment. Depending upon various reasons, locations, and duration, heart failure can be categorized as – acute vs. chronic OR right heart vs. left heart OR systolic vs. diastolic.
Each of these conditions has a distinct clinical presentation and characteristics. Heart failure can occur due to various reasons and risk factors for eg., myocardial injury or infarction, chronic hypertension, valvular dysfunction, arrhythmias, cardiomyopathies, etc. Some of the common symptoms of cardiac heart failure include- shortness of breath, excessive tiredness, and leg swelling. Treatment for heart failure is critically essential and involves the usage of drugs like ACE inhibitors and beta-blockers etc.
Perioperative myocardial injury
Perioperative myocardial injury is a relatively underrecognized, myocardial complication that can occur post- non-cardiac surgery. It should be noted that this condition is characteristically different from myocardial infarction. Patients age ≥ 65 years along with a pre-existing history of atherosclerotic disease are highly predisposed to Perioperative myocardial injury. In this condition, there is a severe increase in plasma concentration of cardiac troponin T (hs-cTn). This condition is often presented and manifested without any chest pain, dyspnea, or other typical cardiac injury symptoms. The absence of most of the classical symptoms often leads to the non-diagnosis of this condition. To rule out the presence of this condition, it is essential to carry out hs-cTn screening perioperatively. Perioperative myocardial injury has been found to significantly increase the risk of 30-day mortality post-noncardiac surgery.
Biological Importance of Myocardium
The heart is the central pumping organ of the body. Contraction and relaxation of the heart result in the pumping of blood throughout the body. For the normal functioning of the body, the cells and tissue need a sufficient amount of oxygen which is supplied by the circulating blood. Cardiac muscles or the myocardium are responsible for the rhythmic and continuous contraction and relaxation i.e. pumping action of the heart. Cardiac muscles are one of the earliest developing embryonic organs that function throughout the life span. These muscles are part of the complex and intricate system of coronary vasculature, cardiac lymphatics, and autonomic innervations. Cardiomyocytes form the thickest layer of the heart walls. Being such a central organ in the body, dysfunction of the myocardium can have a serious outcome. Globally, cardiovascular diseases form the foremost cause of mortality. A number of cardiac diseases involve the myocardium involving, resulting in contractile dysfunction, cell damage and death, and cardiac pump failure.
Try to answer the quiz below to check what you have learned so far about myocardium.
Further Reading
References
- Langer, G. A., Frank, J. S., & Brady, A. J. (1976). The myocardium. International review of physiology, 9, 191–237.
- Edwards B.S. and Edwards J.E. (2007). Myocardial Disease. In: Pathology of Sudden Cardiac Death. Edwards B.S. and Edwards J.E. (Eds). doi:10.1002/9780470988480.ch3.
- Mahadevan, V. (2018). Anatomy of the heart, Surgery (Oxford), 36 (2), 43-47.
- Terracciano, C. and Guymer, S. (2019). Heart of the Matter Key concepts in cardiovascular science: Key concepts in cardiovascular science. 10.1007/978-3-030-24219-0.
- Whitaker, R.H. (2018). Anatomy of the heart. Medicine, 46 (8), 423-426,
©BiologyOnline. Content provided and moderated by BiologyOnline Editors.


