Virulence
n., [ˈvɪɹələns]
Definition: degree to which an organism can cause disease
Table of Contents
Virulence Definition
In biology, virulence is defined as the degree to which a pathogenic organism can cause disease. A related word, virulent, describes a pathogen that is relatively toxic or capable of causing relatively more harm to the health of its host compared with other pathogens. Virulence encompasses various factors and traits that contribute to the severity and harm caused by a pathogen, including its ability to colonize, evade the host’s immune system, and induce damage.
Etymology: The term “virulence” is derived from the Latin word “virulentia,” meaning “poisonous” or “venomous.”
Synonym: disease-causing potential
Variants: virulency
What is the difference between pathogenicity and virulence?
Virulence is related to pathogenicity in the sense that its meaning is correlated to the manifestation of a disease. However, pathogenicity, in particular, is defined as the ability of a pathogen to cause disease. An organism that harms its host and causes the disease is called a pathogen. Thus, a microorganism can be categorized into two based on pathogenicity — whether it is pathogenic or non-pathogenic. The capability to produce disease is associated with the inherent characteristics of the organism in an effort to survive inside the host.
Conversely, virulence refers to the degree of pathogenicity of a particular organism. A virulent pathogen is, therefore, one that causes damage to its host to an extent that is significantly greater than that caused by avirulent (or non-virulent) pathogens.
Pathogenicity vs. Virulence in 2 mins! (by Dr Matt & Dr Mike):
What is an Example of a Virulent?
Human immunodeficiency virus or HIV is an example of a virulent virus. It is the causative agent of AIDS. It is virulent because it employs mechanisms for evading the host immune cells. For instance, it infects the T-helper cell, one of the immune cells. Thus, the immune response of the host is already reduced and compromised.
Another example is lyssavirus, which causes rabies. It enters and hijacks muscle cells, and then travels to the nervous system through the neuromuscular junctions. (Ref.3) Thus, it is particularly described as neurovirulent, i.e. for being able to cause disease in the nervous system.
As for bacteria, examples are the two human pathogens: Mycobacterium tuberculosis (causative agent of tuberculosis) and Bacillus anthracis (causative agent of anthrax).
Virulence Factors
Now that we learned the difference between virulence and pathogenicity, let us now know what makes a pathogen more virulent than the others. The virulence of a pathogen is influenced by different factors that are not solely attributable to the microorganism but to the host and the environment as well.
What is a virulence factor definition?
Pathogenic organisms have a different breadth of virulence. For example, a strain of bacteria may be more virulent than the other strains of the same species. The virulence of a pathogen is often correlated with virulence factors.
A virulence factor is defined as the factor that enables an organism to invade a host and cause disease. It also determines the extent of damage to the host. These factors may be secretory, membrane-associated, or cytosolic in nature.
Key factors include the presence of virulence genes, which encode virulence factors. An example of such a factor is the ability of microbes to multiply within their host cells.
Viral virulence factors, for instance, are chiefly proteins that are incited by the infective virus to be produced by the host’s own protein machinery. Bacterial virulence factors are likewise proteins that are coded for by their own genes or by plasmids that they acquired via horizontal gene transfer.
In microbiology, these factors are considered vital to epidemiology, particularly, when tracking a novel pathogenic strain. That is because the strain is often highly virulent, and therefore more detrimental, even fatal, to its host.
Virulence factors are, therefore, one of the major targets in medical research that intends to create new treatments and vaccines. Some of the virulence factors that researchers look into are the route of entry into its host, the pathobiological machinery employed (e.g., use of adhesins to adhere to host tissues, mechanisms to breach protective membrane barriers, strategies to manipulate host cell processes, etc.) and its effects on the host’s immune response.
Other factors contributing to virulence
The host’s overly reactive immune response may also contribute to the severity of the disease. For instance, when the immune cells are triggered by the presence of these virulence factors, they tend to damage the host cells as well in an effort to counter the infection.
Another external factor is the environmental conditions. Pathogens that are exposed to conditions that are favorable or optimal for their growth, activity, and survival will likely be more virulent. Examples of environmental conditions considered are temperature, humidity, and nutrient availability.
Biological factors can further augment or boost the virulence of a pathogen, e.g., the presence of co-infecting microorganisms, the abundance of vectors, or a wider range of natural reservoirs could enable the ease of transmission.
Measurement Of Virulence
While pathogenicity is a qualitative attribute, virulence is quantitative and thus can be measured.
- Virulence assays, for instance, are used to determine the virulence of a pathogen in a laboratory setting. Factors, such as mortality rates, tissue damage, or the presence of virulence genes, are quantified to gain insights into the virulence of certain strains and their potential to cause outbreaks.
- Virulence factors are used in epidemiology and diagnostics as markers for detecting, identifying, and tracking pathogens.
NOTE IT!
Virulence and Co-Evolution
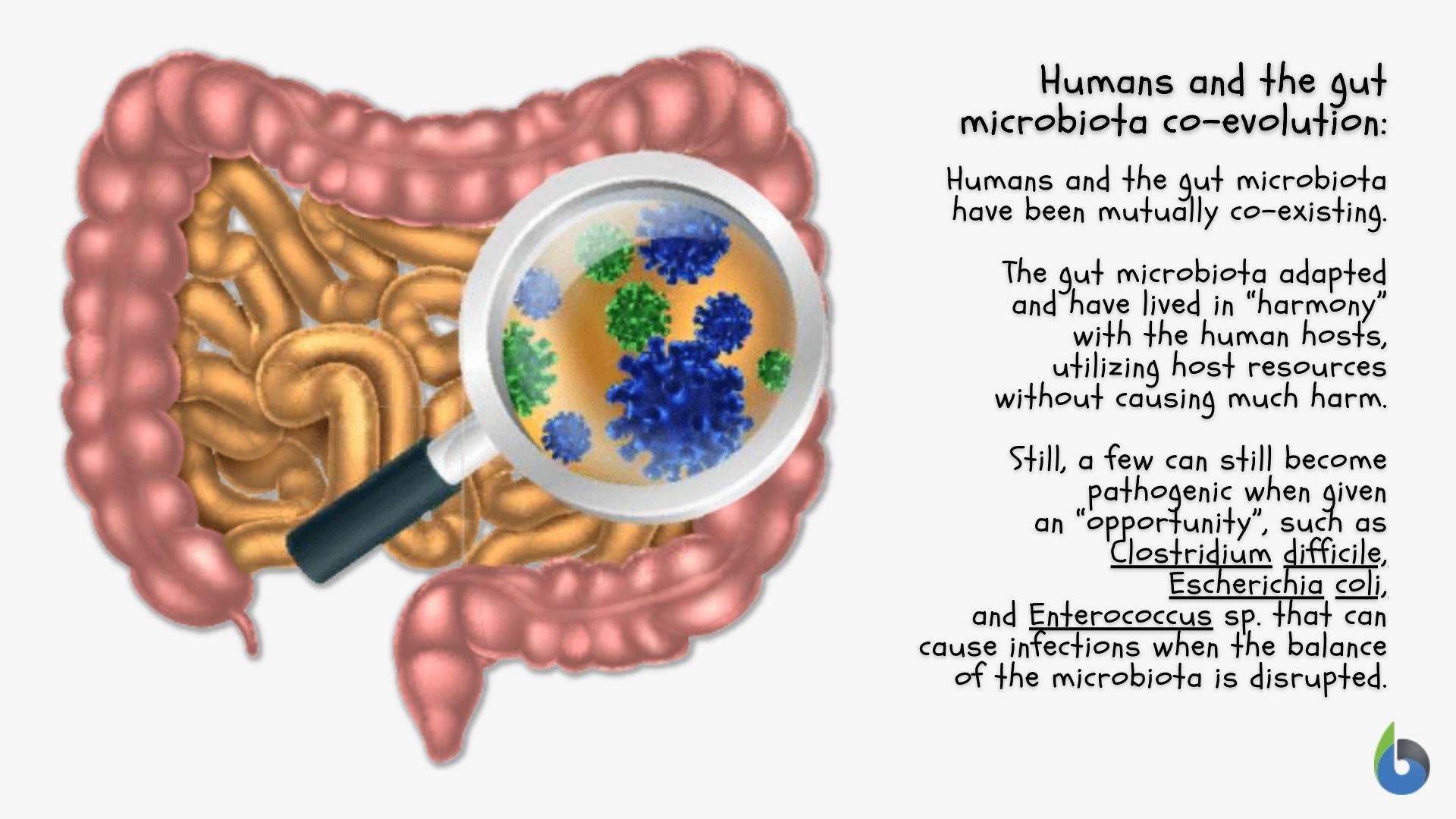
When a microorganism is extremely virulent, one possible reason is it is a novel pathogen of that host. The host as the “new environment” harboring the pathogen may not be equipped to efficiently counter what the novel pathogen is capable of as it establishes its new “home”. Thus, the pathogen would tend to be more “destructive”. But in time, the pathogen will eventually be less detrimental to its host as they co-evolve. In their host-pathogen relationship, while the host may in time develop immunity or tolerance over the pathogen, the pathogen, in turn, may eventually become avirulent or less virulent as they undergo genetic changes that lead to the loss or the attenuation of their virulence factors. A reason that explains how certain pathogens would evolve to be “nicer” to their host is that those that “compromise” rather than “kill” their host would seem to be favored in nature as they tend to tap on their host’s resources for a longer time, thus, persist, over those whose resource opportunities are curtailed due to the resulting demise of their host by their presence.
Take the Virulence – Biology Quiz!
Further Reading
References
- Pathogenicity vs Virulence. (2020). Retrieved from Tulane.edu website: https://www.tulane.edu/~wiser/protozoology/notes/Path.html
- Sharma, A. K., Dhasmana, N., Dubey, N., Kumar, N., Gangwal, A., Gupta, M., & Singh, Y. (2016). Bacterial Virulence Factors: Secreted for Survival. Indian Journal of Microbiology, 57(1), 1–10. https://doi.org/10.1007/s12088-016-0625-1
- Gonzaga, M. V. (2019, May 24). Rabies pathobiology and its RNA virus agent – Lyssavirus – Biology Online Article. Biology Articles, Tutorials & Dictionary Online. https://www.biologyonline.com/rabies-pathobiology-and-its-rna-virus-agent-lyssavirus
©BiologyOnline.com. Content provided and moderated by Biology Online Editors.