Digestion and Absorption of Food
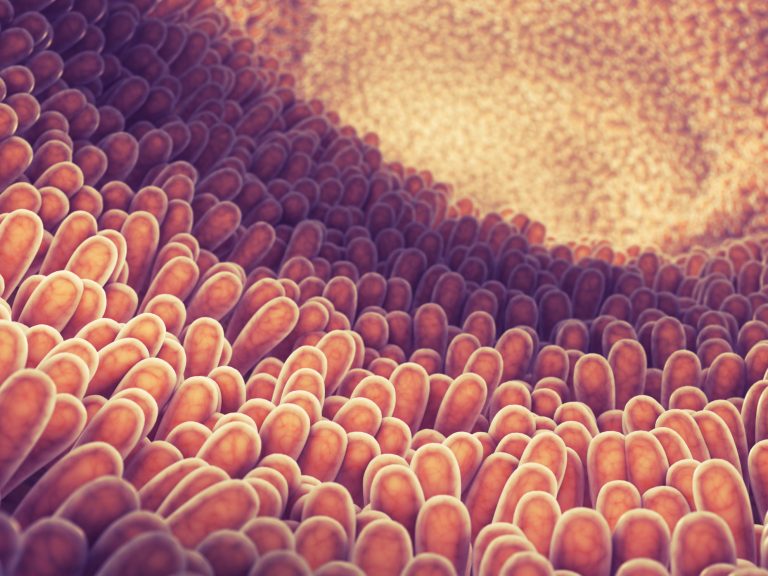
Intestinal villi projecting into the lumen of the small intestine are essential for greater surface area for absorption of digested nutrients.
Table of Contents
The gastrointestinal (GI) system includes the gastrointestinal tract (mouth, pharynx, esophagus, stomach, small intestine, large intestine) and accessory organs (salivary gland, liver, gallbladder, pancreas) that secrete substances into the tract via connecting ducts. GI system breaks down particles of ingested food into molecular forms by enzymes (digestion) that are then transferred to the internal environment (absorption). For the labeled parts of the human digestive system, view here.
Functions of GI organs
The GI tract begins at the mouth, where digestion begins with chewing. Saliva containing mucus and the enzyme amylase is secreted from 3 pairs of salivary glands, located in the head. Mucus moistens the food and amylase partially digests polysaccharides (starches). Food then reaches the stomach through the pharynx and esophagus.
The stomach is the sac that stores and digests food macromolecules into a solution called chyme. Glands lining the stomach secrete hydrochloric acid that dissolves food particles and protein-digesting enzymes, called pepsin.
Final stages of digestion and most of the nutrient absorption occur in the next portion of the tract: the small intestine. The small intestine is divided into 3 segments – duodenum, jejunum, and ileum.
The pancreas is a gland located behind the stomach. From its exocrine portion, it secretes (1) digestive enzymes and (2) a fluid rich in HCO3– ions to neutralize the acid from the stomach. The liver secretes bile. Bile contains HCO3– ions and bile salts to solubilize fats. Bile reaches the gall bladder through hepatic ducts and is stored in the gall bladder between meals. During a meal, bile is secreted from the gland by smooth muscle contraction and reaches the duodenum portion of the small intestine by the common bile duct.
Monosaccharides, amino acids, and mineral salts are absorbed by transporter-mediated processes while fatty acid and water diffuse passively.
Undigested material is passed to the large intestine, where it is temporarily stored and concentrated by reabsorption of salts and water. Finally, contractions of the rectum, the last part of the large intestine, expel the feces through the anus.
Structure of GI Tract Wall
The luminar surface is covered by a single layer of epithelium containing exocrine and endocrine cells. The exocrine cells disintegrate and discharge into the lumen, releasing their enzymes. The epithelia with an underlying layer of connective tissue (lamnia propia) and muscle (muscularis mucosa) are called the mucosa. Below the mucosa is a layer of inner circular and outer longitudinal smooth muscle called muscularis externa, which provides the forces for moving and mixing the GI contents. The outermost layer of the tube is made up of connective tissue called serosa. The luminar surface of the tube is highly convoluted into projections called villi and microvilli; both of which increase the total surface area for absorption. The center of each villus has a single blunt-ended lymphatic vessel called a lacteal. Venous drainage from the intestine transports absorbed materials to the liver for processing via the hepatic portal vein.
Digestion and Absorption
Carbohydrate
Digestion begins in the mouth by salivary amylase and completed in the small intestine by pancreatic amylase. Monosaccharides, such as glucose, galactose, and fructose, are produced by the breakdown of polysaccharides and are transported to the intestinal epithelium by facilitated diffusion or active transport. Facilitated diffusion moves the sugars to the bloodstream.
Protein
Proteins are broken down to peptide fragments by pepsin in the stomach, and by pancreatic trypsin and chymotrypsin in the small intestine. The fragments are then digested to free amino acids by carboxypeptidase from the pancreas and aminopeptidase from the intestinal epithelium. Free amino acids enter the epithelium by secondary active transport and leave it by facilitated diffusion. Small amounts of intact proteins can enter interstitial fluid by endo- and exocytosis.
Fat
Fat digestion occurs by pancreatic lipase in the small intestine. A monoglyceride and two fatty acids are produced in the digestive process. Large lipid droplets are first broken down into smaller droplets, by a process called emulsification. Emulsification is driven by mechanical disruption (by the contractile activity of the GI tract) and emulsifying agents (amphipathic bile salts). Pancreatic colipase binds the water-soluble lipase to the lipid substrate.
Digested products and bile salts form amphipathic micelles. These micelles keep the insoluble products in soluble aggregates from which small amounts are released and absorbed by epithelial cells via diffusion. Free fatty acids and monoglycerides then recombine into triacylglycerols at the smooth ER, are processed further in the Golgi and enter the interstitial fluid as droplets called chylomicrons, which are then taken up by the lacteals in the intestine.
Vitamins
Fat-soluble vitamins are absorbed and stored along with fats. Most water-soluble vitamins are absorbed by diffusion or mediated transport. Vitamin B12, because of its large size and charged nature, first binds to a protein, called intrinsic factor, which is secreted by the stomach epithelium, and is then absorbed by endocytosis.
Water
The stomach absorbs some water but most are absorbed in the small intestine by diffusion.
Regulation of GI Processes
Control mechanisms of the GI system regulate conditions in the lumen of the tract. Reflexes are initiated by:
- Distension of wall by volume of luminal contents
- Chyme osmolarity
- Chyme pH
- Chyme concentrations of specific products.
Neural regulation of the GI tract
Impulses to the GI muscles and exocrine glands are supplied by the enteric nervous system, the local nervous system of the GI tract, which allows local, short reflexes, independent of CNS. Long reflexes through the CNS are possible via sympathetic and parasympathetic nerves, which also innervate the GI tract.
Hormonal regulation
Endocrine cells are scattered throughout GI epithelia and the surface of these cells is exposed to the lumen. Chemical substances in the chyme stimulate them to release hormones into the blood.
Phases of GI control
Each phase is named according to where the receptor for a reflex is located. These phases do not occur in a temporal sequence.
- The cephalic phase is initiated when sight, smell, taste, chewing, and emotional states stimulate receptors in the head. Reflexes mediated by sympathetic and parasympathetic fibers activate secretory and contractile activity.
- The gastric phase is initiated by distension, acidity, and the presence of amino acids and peptides in the stomach. This phase is mediated by short and long reflexes and activates the secretion of gastrin.
- The intestinal phase is initiated by distension, acidity, the osmolarity of digestive products in the intestine and is mediated by GI hormones and short and long neural reflexes.
Mouth, Pharynx, and Esophagus
Chewing is controlled by somatic nerves to the skeletal muscles and the reflex activation of mechanoreceptors on the palate, gums, and tongue.
Autonomic nerves in response to chemoreceptors and pressure receptors in the mouth stimulate saliva secretion.
Swallowing is mediated by pressure receptors on walls of the pharynx, which send impulses to the swallowing center in the medulla oblongata. The center activates muscles in the pharynx and esophagus. Multiple responses occur in a temporal sequence. The palate is elevated to prevent food from entering the nasal cavity, respiration is inhibited and the epiglottis covers the glottis to prevent food from entering trachea (windpipe). The upper esophageal sphincter opens and food enters the esophagus and moves toward the stomach by muscle contractions called peristaltic waves. Food then moves to the stomach when the lower esophageal sphincter opens. A less efficient, or faulty, lower esophageal sphincter results in the reflux of gastric contents into the esophagus (gastroesophageal reflux), this reversal results in heartburn and over time contributes to ulceration of the esophagus.
Epithelium lining the stomach invaginates into the mucosa, forming tubular glands. Parietal (oxyntic) cells secrete acid and intrinsic factor and chief cells secrete pepsinogen. Also scattered throughout are enterochromaffin-like (ECL) cells, which secrete histamine, and other cells that secrete somatostatin. The antrum, a lower portion of the stomach, secretes gastrin.
Increased protein content in a meal stimulates the release of gastrin and histamine, which in turn stimulates HCl secretion. Somatostatin inhibits acid secretion by inhibiting the release of gastrin and histamine. Enterogastones in the duodenum also inhibit gastric acid secretion. The precursor pepsinogen, which is produced by chief cells, is converted to pepsin by the acid in the stomach.
The stomach produces peristaltic waves in response to the arrival of food. The pyloric sphincter between the stomach and duodenum opens to release small amounts of chyme into the duodenum with each wave. These waves are generated by pacemaker cells in the longitudinal smooth muscle layer and are spread out by gap junctions. Gastrin, distension of the stomach, etc. stimulate gastric motility while distension of duodenum inhibits it.
Pancreatic Secretions
Inactive trypsinogen is secreted by the pancreas and is later converted by the intestinal enzyme enterokinase to active trypsin, which digests proteins. Pancreatic amylase and lipase are secreted in active forms. The pancreas also secretes bicarbonate ions.
The secretion of pancreatic enzymes is stimulated by cholecystokinin (CCK), the secretion of which is triggered by the detected presence of fatty acids and amino acids in the small intestine. The secretion of bicarbonate ions is stimulated by secretin, which is triggered by acidity in the small intestine.
Bile Secretion
Bile contains bile salts, which solubilize fats, and bicarbonate ions, which in turn are used to neutralize stomach acids. Bile salts, secreted by hepatocytes (liver cells) enter the GI tract and are reabsorbed by transporters in the intestine and are returned to the liver via the portal vein. This recycling pathway is called the entero-hepatic circulation.
The sphincter of Oddi controls the entry of the bile duct into the duodenum. When the sphincter is closed, the secreted bile is shunted into the gallbladder. The presence of fat in the intestine releases CCK, which relaxes the sphincter to discharge bile salts into the duodenum.
Small Intestine
The most common motion of the small intestine is stationary contraction and relaxation, called segmentation. Segmentation results in little net movement. The chyme is mixed and brought into contact with the intestine wall and then moved slowly toward the large intestine. The movements are initiated by pacemaker cells in the smooth muscle layer.
After most of the materials are absorbed, segmentation is replaced by a peristaltic activity called the migrating motility complex, which moves any undigested material to the large intestine. The candidate intestinal hormone, motilin, initiates migrating motility.
Large Intestine
The large intestine consists of 3 parts: the cecum, colon, and rectum. The primary function is to store and concentrate fecal material for elimination. Chyme enters the cecum through the ileocecal sphincter, which relaxes and opens as a result of the gastroileal reflex.
Na+ is absorbed along with water. K+ and HCO3– ions are secreted into the lumen. Undigested polysaccharides (fiber) are metabolized to short-chain fatty acids by the residing bacteria and these are then absorbed by diffusion. A small amount of vitamin K is also produced and absorbed. Bacterial metabolism produces a mixture of gases, called flatus.
Motility and Defecation
Regular contractions of the circular smooth muscle produce a slow rhythmic segmentation movement. The undigested material moves slowly in order to provide resident bacteria time to grow and multiply. Following a meal, there is a wave of intense contraction, called mass movement. The internal anal sphincter is made of smooth muscle and closes the anus, while the external anal sphincter is made of skeletal muscle and is under voluntary control. Both sphincters regulate the anal opening and closing. Mass movement of fecal material into the anus initiates the defecation reflex, which is mediated by mechanoreceptors. The two sphincters open to expel the feces. If defecation is delayed, rectal contents are driven back into the colon by reverse peristalsis until the next mass movement.
Pathophysiology of the GI Tract Ulcers
Ulcers are eroded areas of gastric surface and breaks in the mucosal barrier, which expose the underlying tissue to the corrosive action of acid and pepsin. Damage to underlying blood vessels may cause bleeding.
Vomiting
The vomit reflex results in the forceful expulsion of toxic gastric contents. This reflex is coordinated by the vomiting center in the medulla oblongata. Various mechano- and chemoreceptors in the stomach and elsewhere can trigger this reflex. Increased salivation, sweating, heart rate, pallor, etc. accompany the reflex. Abdominal muscles contract to raise abdominal pressure while the lower esophageal sphincter opens and gastric contents are forced into the esophagus (retching). If the upper esophageal sphincter opens, contents are then expelled from the mouth (vomiting). Excessive vomiting can lead to loss of water and salts, which will ultimately result in dehydration.
Gallstones
Excessive secretion of water-insoluble cholesterol in bile results in the formation of crystals, called gallstones, which can close the opening of the gallbladder or the bile duct. If a stone prevents bile from entering the intestine fat digestion and absorption decreases. If a stone blocks the entry of the pancreatic duct, it prevents pancreatic enzymes from entering the intestine, thus preventing the digestion of other nutrients. A blocked bile duct inhibits the further secretion of bile, resulting in the accumulation of bilirubin in tissues, producing a yellowish coloration called jaundice. Jaundice is common in newborns and is rectified by sunlight exposure.
Lactose Intolerance
Lactose intolerance results from a lack of the enzyme lactase which digests lactose, the sugar in milk. The lack of lactase results in the incomplete digestion of lactose to glucose and galactose.
Constipation and Diarrhea
Constipation is the absence of defecation due to decreased motility of the large intestine. This results in excess absorption of water from feces, making it hard to expel.
Dietary fiber, which is not digested in the small intestine, can produce distension and increase motility.
Diarrhea results from decreased fluid absorption, or increased fluid secretion resulting in an increased luminal fluid, which in turn, causes distension and increased motility. Diarrhea results in decreased blood volume, loss of water, and other nutrients.
Further Reading
- Digestive enzymes – Science Learning Hub. (Know the different digestive juices and enzymes through this article).
You will also like...
Digestion and Absorption of Food
The gastrointestinal system breaks down particles of ingested food into molecular forms by enzymes through digestion and..
Plant Auxins – Phototropism & Geotropism
Plants produce hormones to regulate their growth. Auxins, for instance, influence plant growth. Know the role of auxin i..

Abiotic Factors – Water Conditions
A still body of water may be disturbed by a variety of factors. One of them is wind. In fact, it is considered as the pr..

Genetics – Lesson Outline & Worksheets
Topics Modules Quizzes/Worksheets Description Introduction to Genetics Genetics – Definition: Heredity and ..
Mendel’s Law & Mendelian Genetics
One of Mendel’s law of inheritance is the “law of dominance”. Read this tutorial to know more about this form of i..

Developmental Biology
Developmental biology is a biological science that is primarily concerned with how a living thing grows and attains matu..
