Human Reproduction
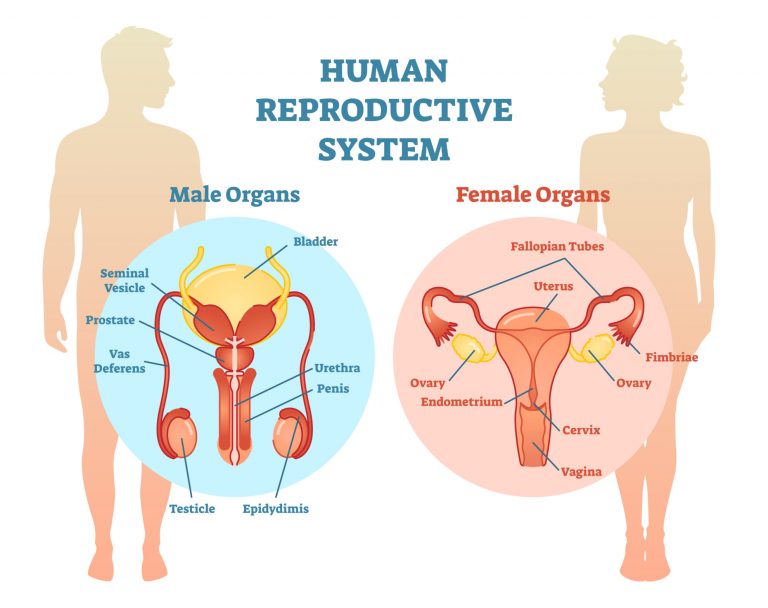
Male and female reproductive systems
Table of Contents
Terminology and Concepts
Primary reproductive organs are called gonads – testes in the male and ovaries in the female. Gonads (1) produce reproductive cells called gametes – spermatozoa in males and ova in females, the process is called gametogenesis, and (2) secrete steroid hormones called sex hormones – testosterone in male, estradiol, and progesterone in females.
Testosterone belongs to a class of hormones that have masculinizing actions called androgens and estradiol belongs to a class of hormones called estrogens. Androgens are not unique to males and estrogens are not unique to females.
GnRH stimulates the release of pituitary gonadotropins – FSH and LH, which act upon the gonads to stimulate the development of sperm and ova and secretion of sex hormones. The sex hormones exert negative feedback on the secretion of GnRH, LH, and FSH.
Accessory reproductive organs consist of ducts through which sperm and ova are transported and the glands emptying into these ducts. Secondary sexual characteristics comprise the external differences between males and females.
Gametogenesis
Developing gametes are called germ cells and the first stage in their development is the proliferation of primordial germ cells by mitosis or cell division in which each daughter cell receives a full set of chromosomes identical to those of the original cell. In females, this mitotic activity occurs only during embryonic development while in males it begins at puberty and continues throughout life. Although this is currently an area of research and new things are coming to light with regards to mitotic activity in female gonads. The second stage of development occurs by meiosis or cell division in which each daughter cell receives half of the chromosomes of the original cell.
Male Reproductive Physiology
Testes are suspended in sacs called the scrotum. Spermatogenesis or sperm formation occurs in seminiferous tubules in the testes. Walls of these tubules are composed of developing germ cells, Sertoli cells and Leydig cells that lie between the tubules secrete testosterone. Seminiferous tubules empty into a duct called the epididymis, which leads to the vas deferens. Ducts from the two glands – the seminal vesicles join the vas deferens to form two ejaculatory ducts, which then enter the prostate gland and the paired bulbourethral glands before joining the urethra. Prostate glands and seminal vesicles secrete a fluid in which sperm cells are suspended, and this fluid together with the sperm cells is called semen. The glandular secretions contain nutrients, buffers that protect the sperm from vaginal acidity, chemicals that increase sperm motility and mucus for lubrication.
Spermatogenesis
Undifferentiated germ cells, termed spermatogonia, divide by mitosis and differentiate to produce primary spermatocytes, which grow and undergo first meiotic division to form secondary spermatocytes, which undergo second meiotic division to form spermatids. Spermatids then develop into spermatozoa.
The head of a sperm consists of DNA nucleus and a tip, which is covered by the acrosome, a vesicle containing many enzymes that play an important role in sperm’s penetration of egg. Most of the tail is a flagellum that propels the sperm.
Leydig cells secrete testosterone and Sertoli cells divide the tubules into separate compartments with separate environments where different stages of spermatogenesis can take place. They also secrete androgen binding protein, which binds testosterone and act as intermediaries between germ cells and hormones.
Sperm Transport
The vas deferens and epididymis store the sperm until ejaculation. Sperms are non-motile at this time. During passage through the epididymis, they are concentrated by fluid absorption.
Erection
The penis consists of vascular compartments and arteries supplying them are normally constricted so that there is little blood in them, and the penis is flaccid. Sexual excitation in higher brain centers, stimulation of mechanoreceptors in the penis, inhibition of sympathetic fibers and release of nitric oxide dilate these arteries, cause these compartments to become engorged with blood at high pressure, making the penis elongated and rigid. Erectile dysfunction is the inability to achieve an erection due to various physiological and/or psychological causes. Viagra, and related products, block the breakdown of cGMP; a messenger involved in the relaxation of arterial smooth muscle, which promotes erection.
Ejaculation
Stimulation of sympathetic nerves contracts the smooth muscles lining the ducts and discharges semen through urethra. The sphincter at the base of the urinary bladder is closed so that sperm cannot enter the bladder nor can urine be expelled. Heart rate and blood pressure increase and skeletal muscles contract throughout the body and this event is called orgasm.
Hormonal control of male reproductive functions
- FSH: acts on Sertoli cells to stimulate spermatogenesis.
- LH: acts on Leydig cells to stimulate testosterone secretion.
- Testosterone: Stimulates spermatogenesis, induces differentiation of male accessory reproductive organs and maintains their function, induces male secondary sex characteristics, stimulates protein anabolism, bone growth, erythropoietin secretion, and required for sex drive and may enhance aggressive behavior.
Female Reproductive Physiology
Production of the female gamete, the egg, followed by its release from the ovary is called ovulation. Ovulation is cyclical and predictable. These cycles are called menstrual cycles in humans. Cyclical changes in hormone secretion by ovaries cause changes in the entire female reproductive tract, including the uterus, which is made ready to receive and nourish the gamete. There is no menstruation during pregnancy.
The ovaries end close to the uterine tubes (oviducts or fallopian tubes), which are attached to the uterus. The uterus is a hollow, thick-walled, muscular organ that houses the fetus during pregnancy and is the source of bleeding during menstruation. The lower portion of the uterus is called the cervix, and the canal leading from the cervix to the outside is the vagina. These are the structures of the female internal genitalia.
Ovarian function
Oogenesis. Primitive germ cells, called oogonia undergo mitosis and develop into primary oocytes (with 46 chromosomes) and remain at a state of meiotic arrest (they begin the first meiotic development but do not complete it). All the germ cells in a female are at this developmental stage at birth. Although this is an area currently being studied further.
At puberty, primary oocytes destined for ovulation complete meiosis, each daughter cell receiving 23 chromosomes. One of the two daughter cells retains all the cytoplasm and is called the secondary oocyte while the other, called the first polar body, is nonfunctional. The second meiotic division occurs in the uterine tube after ovulation, ONLY IF the secondary oocyte is fertilized. Again, one daughter cell retains all the cytoplasm and is called ovum while the other cell, called the second polar body, is nonfunctional and is later absorbed by the body.
Control of ovarian function
Three Phases: (1) Follicular Phase of Ovary (corresponding to the Proliferative Phase of the Uterus), (2) Luteal Phase of Ovary (corresponding to Secretory Phase of the Uterus), and (3) Beginning of new cycle (corresponding to Menstrual Phase of the Uterus).
- Follicular Phase of Ovary. FSH and LH increase during the follicular phase because estrogen concentration is low and therefore negative feedback on these pituitary hormones is low. FSH and LH stimulate primary follicles (containing primary oocytes) to grow and stimulate their theca cells to produce estrogen. Estrogen leads to a thickening of the uterine epithelium, the endometrium. Estrogen begins to exert a negative feedback on FSH. As FSH goes down, all the follicles cannot be maintained and all but one follicle degenerates. The one dominant follicle (Graafian follicle) survives because (a) it is hyperresponsive to FSH and can maintain itself even under low FSH, and (b) it also becomes sensitive to LH. In the meanwhile, LH does not drop but shoots up (LH surge) because increased estrogen exerts a positive feedback effect on the LH releasing mechanism of the pituitary. LH surge leads to the release of the primary oocyte (ovulation).
- Luteal Phase of Ovary. The now-empty follicle, corpus luteum, starts secreting estrogen and progesterone. These hormones exert a negative feedback on secretion from LH and FSII, preventing new follicles from maturing. Progesterone converts the endometrium into a secretory tissue full of glycogen and blood vessels, ready to receive a fertilized egg.
- Beginning of new cycle. (If the egg is not fertilized) If fertilization does not occur, the corpus luteum degenerates and estrogen and progesterone levels recede. The lack of estrogen and progesterone leads to the collapse of the vascular endometrium, which in turn leads to menstruation.
Pregnancy
Egg and Sperm Transport. At ovulation, the egg enters the uterine tube. Sperm enters the uterus during intercourse and moves into the uterine tube through its own rhythmic propulsions. Most of the sperm cells die in the acidic vaginal environment and/or due to the exhaustion of their energy supply.
Fertilization. The sperm binds to the egg by complementary surface proteins. The binding triggers the acrosome reaction in the sperm and its enzymes digest the egg membrane. The sperm then passes into the cytoplasm of the egg. The fertilized egg (zygote) releases enzymes that harden the egg membrane and inactivate the sperm binding sites to prevent additional sperms from fusing.
Implantation and Placentation. The zygote undergoes mitotic cell divisions (without cell growth) called cleavage, becoming a blastocyst, which embeds in the endometrium, in a process called implantation. If the zygote divides into two completely separate masses, it results in identical (monozygotic) twins. Fraternal twins result from two ovulated eggs being fertilized. The outer layer of the blastocyst, the trophoblast gives rise to the fetal part of the placenta while the inner cell mass develops into the embryo proper. Fetal blood and maternal blood both flow through the placenta (without mixing), exchanging gases, nutrients, hormones, and wastes through a structure called the placenta. The placenta is a combination of fetal and maternal tissues. Blood vessels enter and leave the placenta through the umbilical cord, which is connected, to the baby at the site of the belly button. The fetus is surrounded by a space called the amniotic cavity filled with a fluid called amniotic fluid, providing a buffer to mechanical and other disturbances. A number of genetic disorders can be diagnosed by sampling this amniotic fluid (amniocentesis) for the presence or absence of certain chemicals.
Hormonal Changes during Pregnancy. The uterus is maintained during pregnancy by progesterone and estrogen that initially comes from the corpus luteum, which in turn is maintained by the hormone, chorionic gonadotropin that is produced by the trophoblast. Corpus luteum later regresses and the placenta itself produces the required estrogen and progesterone. High levels of these hormones inhibit the secretion of GnRH and gonadotropins, thus eliminating menstrual cycles during pregnancy.
Parturition. A normal pregnancy lasts for 38 weeks from the day of ovulation and conception. Delivery occurs by rhythmical contractions of the uterus, stimulated by oxytocin. The cervix dilates and the infant moves out through the vagina.
Lactation. Lactation is the secretion of milk by the mammary glands, or breasts. Estrogen and progesterone secretion at the onset of puberty leads to breast enlargement due to the development of the duct system. During pregnancy, estrogen stimulates the secretion of prolactin and placental lactogen, which stimulate the development of the glands (alveoli) in the breasts. However, milk secretion is inhibited by estrogen and progesterone during pregnancy. A decline in the levels of these two hormones as a result of placental removal during childbirth removes the inhibitory effect. Milk secretion is maintained by prolactin release as a result of afferent input from nipple receptors to the hypothalamus during suckling which also inhibits dopamine secretion. Milk ejection from the alveoli to the ducts is stimulated by the action of oxytocin, released as a result of the suckling reflex. Suckling also inhibits the hypothalamo-pituitary-ovarian hormone chain, which in effect blocking ovulation.
Contraception
Oral contraceptives are made of synthetic progesterone and estrogen combinations that inhibit pituitary gonadotropin release and thereby prevent ovulation. Postcoital contraceptives include progesterone antagonists that prevent progesterone from binding to the uterine wall, leading to erosion of the endometrium.
Puberty
Puberty is the period during which reproductive organs mature and reproduction becomes possible. This process is initiated by the secretion of adrenal androgens which is stimulated by ACTH. In females, the first menstrual period is called menarche.
Menopause
Menopause is the cessation of menstrual periods with age, as a result of a decrease in the number of ovarian follicles and their hyporesponsiveness to gonadotropins. Plasma estrogen levels decrease resulting in high gonadotropin secretion. A decrease in bone mass called osteoporosis occurs as well as hot flashes or the sudden dilation of arterioles, an increase in body temperature, and sweating.
You will also like...

Growth Patterns
This tutorial describes the sigmoid curve, annual plant growth, tree growth, human growth, and insect growth as the grow..
Biological Cell Defense
Organisms employ different strategies to boost its defenses against antigens. Humans have an immune system to combat pat..

Vascular Plants: Ferns and Relatives
Ferns and their relatives are vascular plants, meaning they have xylem and phloem tissues. Because of the presence of va..

Independent Assortment and Crossing Over
This tutorial describes the independent assortment of chromosomes and crossing over as important events in meiosis. Read..
New Zealand’s Unique Geographical History
Explore why New Zealand has such unique flora and fauna, and learn why long periods of geographical isolation. This less..
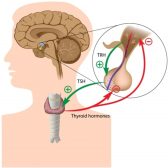
Hormone Production
Hormones are chemical messengers produced by specialized glands and they were produced by switching on the genes designe..
