Kidneys and Regulation of Water and Inorganic Ions

Kidneys regulate water and inorganic ions
Table of Contents
Renal Functions
Kidneys remove/add substances from/to the plasma.
- Regulate water concentration, inorganic ion composition, and volume of the internal environment by controlling their excretion.
- Excrete metabolic wastes, including urea, uric acid, and creatinine into urine
- Excrete foreign chemicals in urine
- Synthesize glucose from amino acids and other precursors (gluconeogenesis).
- Secrete the hormones, erythropoietin, renin, and 1, 25-dihydroxyvitamin D3.
Structure of Kidneys and Urinary System
The two kidneys lie near the back of the abdominal wall. Urine flows from kidneys through ureters into the bladder, from which it is eliminated through the urethra. The outer part of the kidney is called the renal cortex and the inner part is called renal medulla. Each kidney is made up of subunits called nephrons and each nephron consists of (1) an initial filtering component called renal corpuscle located in the cortex and (2) a tubule located in the medulla that extends out from renal corpuscle. The renal corpuscle forms a filtrate that is free of cells and proteins, and as it flows through the tubule, substances are added to it or removed from it and the final exiting fluid is called urine.
Each renal corpuscle contains a tuft of capillary loops called glomerulus, which protrudes into a fluid-filled space called Bowman’s space. Blood enters the glomerulus by an afferent arteriole and leaves it by an efferent arteriole. Protein free fluid from glomerulus enters Bowman’s space and is drained by the proximal tubule which leads to the descending limb of the loop of Henle, from where the fluid goes to the ascending limb and then to the distal convoluted tubule. The fluid then flows into the collecting duct system, comprised of the connecting tubule, followed by the cortical collecting duct and the medullary collecting duct. Medullary collecting ducts from numerous nephrons merge and drain into the renal pelvis, which is continuous with the ureter. The tubules are also connected to another set of blood vessels called peritubular capillaries.
The part of ascending limb passing between the afferent and efferent arterioles has a patch of cells called macula densa and wall of the afferent arteriole at this point has cells called juxtaglomerular (JG) cells, which secrete the hormone renin. These two types of cells comprise the juxtaglomerular apparatus (JGA).
Basic Renal Processes
Filtration of plasma from glomerular capillaries into Bowman’s space is called glomerular filtration and the filtrate is called glomerular filtrate. During its passage through tubules, substances move from tubules to peritubular capillaries, a process called tubular reabsorption and substances move from peritubular capillaries to tubules, a process called tubular secretion.
AE = AF + AS – ARA
where
AE = Amount excreted
AF = Amount filtered
AS = Amount secreted
ARA = Amount reabsorbed
For a given substance, a particular combination of all these processes applies.
Glomerular filtration
Glomerular filtrate contains all plasma substances in the same concentrations as plasma except proteins and molecules bound to these proteins. It is a bulk flow process.
Net glomerular filtration pressure = PGC – PBS – πGC
Where:
PGC is glomerular capillary hydrostatic pressure favoring filtration from capillary to Bowman’s space
PBS is Bowman’s space hydrostatic pressure favoring movement from Bowman’s space to capillaries
πGC is osmotic pressure resulting from the presence of protein in glomerular capillary plasma and no protein in Bowman’s space
Normally, net filtration pressure is positive.
Glomerular Filtration Rate (GFR) – Volume of liquid filtered from glomeruli into the Bowman’s capsule per unit time. GFR is determined by net filtration pressure, the permeability of the corpuscular membranes and surface area available for filtration. GFR is subject to physiological regulation by neural and hormonal inputs to afferent and efferent arterioles. Constriction of afferent arterioles decreases PGC while constriction of efferent arterioles increases it. Mesangial cells, which are modified smooth muscle cells are involved in this constriction process.
The filtered load is the total amount of any nonprotein substance filtered into Bowman’s space. It is given by multiplying GFR with the plasma concentration of the substance. If the quantity of a substance excreted in urine is less than filtered load, tubular reabsorption has occurred, if it is more then tubular secretion has occurred.
Tubular reabsorption
Waste products are reabsorbed incompletely so that they are mostly excreted in the urine, while useful products are reabsorbed completely so that they are mostly not excreted.
Reabsorption by mediated transport is responsible for reabsorption of many substances, e.g., glucose molecules are coupled to the reabsorption of sodium. The limit to which these mediated transport systems can move materials per unit time is called transport maximum (Tm). This limit is a result of the saturation of binding sites on membrane transport proteins. In people with diabetes mellitus, plasma glucose concentration is so high that the filtered load of glucose exceeds the glucose Tm. and therefore, glucose appears in urine (glucosuria).
Tubular secretion
Tubular secretion is responsible for moving substances, e.g., H+ and K+ ions, from peritubular capillaries into tubular lumen by diffusion or transcellular mediated transport. Some of the movements are coupled to reabsorption of Na+ ions.
Tubule cells can synthesize glucose, ammonia, etc. and add it to blood as needed. It can catabolize peptides etc. and remove them from the body.
Regulation
Hormones and neurotransmitters regulate channels and transporters. In order to excrete waste products, GFR must be large resulting in large filtered loads of substances. The primary role of the proximal tubule and loop of Henle is to reabsorb large quantities of substances. Such extensive reabsorption ensures that distal segments receive small amounts of substances and that their quantities in urine can be fine-tuned and regulated. Most homeostatic controls are therefore exerted on distal segments.
Renal clearance
Renal clearance is the measure of the volume of plasma from which a substance is completely removed by kidneys per unit time.
Clearance of substance S = (Mass of S excreted per unit time)/Plasma concentration of S
CS = (USV)/PS
Where:
CS = clearance of S
US = urine concentration of S
V = urine volume per unit time
PS = plasma concentration of S
CS of a substance equals GFR if it is filtered but not reabsorbed, secreted or metabolized.
Micturition
Urine flow through ureters to the bladder is propelled by contractions of ureter wall smooth muscle. Urine is stored in the bladder and ejected during urination or micturition. The bladder is a chamber with walls made of smooth muscle called detrusor muscle, contraction of which produces urination. Part of the muscle at the base of the bladder, where urethra begins, functions as a sphincter called the internal urethral sphincter. Below this sphincter is a ring of skeletal muscle called the external urethral sphincter, which surrounds the urethra.
The detrusor muscle receives parasympathetic input, while the internal sphincter receives sympathetic input and the external sphincter receives motor input. While the bladder is filling, there is little parasympathetic input to the detrusor muscle but there are strong sympathetic and motor inputs to the sphincters. While filling occurs, the detrusor muscle is relaxed, and sphincters are closed. As the bladder fills, stretch receptors stimulate the parasympathetic fibers, resulting in contraction of the detrusor muscle. Sympathetic and motor inputs to sphincters are inhibited and sphincters open to produce urination. There is voluntary control over the external sphincter.
Total Body Balance of Sodium and Water
Water is gained from:
- Ingestion
- Oxidation of organic nutrients.
Water is lost from
- Skin via sweat glands
- Respiratory passageways
- Gastrointestinal tract
- Urinary tract
Water and salt balance is primarily a result of regulation through urinary loss.
Basic renal processes for sodium and water
Sodium and water filter freely from glomerular capillaries to the Bowman’s space. They undergo considerable reabsorption in the proximal tubule but the major hormonal controls on reabsorption are exerted in the collecting ducts. They are not secreted into the tubules.
Primary Active Sodium Reabsorption. Sodium moves out of lumen into the epithelium by diffusion or by ion channels or by cotransport with glucose (which is also being reabsorbed) or countertransport with H+ ions (which are being secreted). Na+/K+-ATPase transports sodium out of the epithelium into the interstitial fluid.
Coupling of Water Reabsorption. The removal of sodium lowers the osmolarity of the lumen and raises that of the interstitial fluid. This causes a net diffusion of water from the lumen into the interstitial fluid through the epithelium. Water permeability of the proximal tubule is high but only that of collecting ducts is under the control of vasopressin (ADH). ADH stimulates the insertion of aquaporin channels, increasing water permeability. Low ADH leads to water diuresis or diabetes insipidus. Increased urine flow due to increased solute excretion is called osmotic diuresis.
The Countercurrent Multiplier System
Fluid from proximal tubule has the same osmolarity as plasma since it absorbs sodium and water equally. In the ascending limb, sodium, but not water, is actively reabsorbed from the lumen, making the interstitial fluid of the medulla hyperosmotic. Due to this hyperosmocity, there is passive diffusion of water from the lumen into the interstitial fluid in the descending limb. Fluid in the distal tubule becomes progressively dilute as sodium is transported out and then in the cortical and medullary ducts, water diffuses out of the tubule into the hyperosmotic interstitial fluid and urine is concentrated.
Renal Sodium Regulation
Since sodium is the major extracellular solute, changes in total body sodium result in changes in the volume of extracellular fluid, changing plasma volume and therefore blood pressure, which is detected by the baroreceptors.
Sodium excreted = Sodium filtered – Sodium reabsorbed
Lower total body sodium can decrease GFR by vasoconstriction, resulting in lower pressure in renal arteries. The control of reabsorption is more important for long-term regulation. Aldosterone stimulates sodium reabsorption by cortical collecting ducts (and large intestine, sweat, and salivary glands). The secretion of aldosterone is controlled by angiotensin II, which is produced from angiotensinogen in a reaction, the rate-limiting step of which is controlled by renin from JG cells. These cells act as internal baroreceptors as well as receive sympathetic inputs from external baroreceptors. Angiotensin II is also a vasoconstrictor itself.
Renal Water Regulation
Water excreted = Water filtered – Water reabsorbed
Water excretion is regulated mainly at the level of reabsorption by vasopressin.
- Baroreceptor control of vasopressin secretion. The secretion of vasopressin can be triggered by decreased extracellular volume but the baroreceptor reflex plays a relatively lesser role because it has a higher threshold.
- Osmoreceptor control of vasopressin secretion. Changes in total body water with which there is no change in total body sodium are regulated by reflexes that alter water excretion without altering sodium excretion. Receptors that control vasopressin secretion mainly due to water gain or loss are the osmoreceptors in the hypothalamus.
- Thirst. Stimulated by lower extracellular volume, higher plasma osmolarity, angiotensin II and the brain centers for thirst are located in the hypothalamus.
Potassium Regulation
Potassium is filtered in the renal corpuscle and most of it absorbed in the tubules. Any changes in potassium excretion, however, are mainly due to changes in potassium secretion by cortical collecting ducts. This secretion is associated with reabsorption of sodium by Na, K-ATPase. Aldosterone-secreting cells are sensitive to potassium concentration of their extracellular fluid and an increased potassium concentration stimulates aldosterone production, thereby increasing potassium secretion and its excretion from the body.
Calcium Regulation
In addition to the gastrointestinal tract and kidneys, which determine net intake and excretion of calcium, calcium can be redistributed between extracellular fluid and bone.
- Kidneys. Calcium is filtered in the renal corpuscle and most of it is reabsorbed. There is no tubular secretion of calcium. Therefore, Calcium excreted = Calcium filtered – Calcium absorbed Control of calcium excretion is exerted mainly on reabsorption.
- Gastrointestinal tract. Calcium absorption in the GI tract is under hormonal control and is a major means for control of calcium balance.
- Hormonal Controls:
- Parathyroid hormone. Parathyroid hormones are produced by parathyroid glands in the neck that are controlled directly by extracellular calcium concentration. It increases the movement of calcium from bone tissue into the extracellular fluid, increases renal tubular calcium reabsorption and stimulating the production of 1, 25-dihydroxy-vitamin D3.
- 1, 25-dihydroxyvitamin D3. 1, 25-dihydroxy-vitamin D3 is derived from vitamin D in the liver and kidneys, this hormone increases intestinal absorption of calcium.
- Calcitonin. Parafollicular cells of thyroid gland secrete calcitonin; it decreases plasma calcium concentration by reducing bone resorption.
Hydrogen Ion Regulation
Hydrogen ions can be redistributed in the body by binding it reversibly with a buffer such as bicarbonates, phosphates, proteins and Hb.
- Respiratory Mechanisms. Ventilation is altered by reflex mechanisms in order to compensate for H+ ion imbalance.
- Renal Mechanisms. Kidneys compensate for H+ ion imbalance by altering plasma HCO3– ion concentration. A lowering of plasma H+ ion concentration results in excretion of large quantities of HCO3– ions while a rise in H+ ion concentration results in the production of HCO3– ions and their addition to plasma by tubular cells.
Bicarbonate Handling
HCO3– is filtered at the renal corpuscle and undergoes reabsorption in the tubule. It is also secreted in the collecting ducts. Therefore:
HCO3– excreted = HCO3– filtered + HCO3– secreted – HCO3–reabsorbed
Inside the cell, CO2and H2O combine to form H2C03, which dissociates to yield H+ and HCO3-ions. HCO3-moves to the interstitial fluid by diffusion while H+ ion is secreted into the lumen by an active process involving H-ATPase pumps. The secreted H+ ion combines with filtered HCO3– in the lumen and generates CO2 and H2O, which diffuse into the cell and the whole process is repeated. If an excess of H+ ions is secreted, it combines with nonbicarbonate buffer, usually HPO4-2, in the lumen and is excreted. In such a case, the HCO3– generated within the cell and entering the plasma is a net gain of HCO3–.
More worksheets:
You will also like...
New Zealand’s Unique Geographical History
Explore why New Zealand has such unique flora and fauna, and learn why long periods of geographical isolation. This less..

Sensory Systems
A sensory system is a part of the nervous system consisting of sensory receptors that receive stimuli from the internal ..
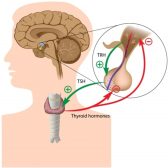
Hormone Production
Hormones are chemical messengers produced by specialized glands and they were produced by switching on the genes designe..
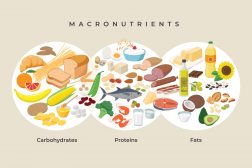
A Balanced Diet – Carbohydrates and Fat
Apart from vitamins, the human body also requires high energy sources such as carbohydrates and fats. If you want an ove..

Inheritance and Probability
Gregor Mendel, an Austrian monk, is most famous in this field for his study of the phenotype of pea plants, including ..

Gene Action – Operon Hypothesis
Learn how the way genes control and determine every aspect of the body. This lesson uses lac operon as an example. ..
..
