Muscle
The human muscle are comprised of cells specialized for generating force and movement
Table of Contents
Muscle cells are specialized to generate force and movement. There are three types of muscle tissue: (1) skeletal muscle, (2) smooth muscle, and (3) cardiac muscle.
Skeletal Muscle
Attached to the bone and moves them by contraction. The contraction is initiated by neural impulses and is under voluntary control.
Structure
A muscle consists of a number of muscle fibers bound together by connective tissue and it is attached to a bone by collagen bundles called tendons. A single muscle fiber is a multinucleated cell and is formed from myoblasts during development. After infancy, new fibers are formed only from undifferentiated satellite cells and any compensation for lost muscles in adulthood occurs mostly through an increase in the size of fibers. Skeletal muscle cells have longitudinal bundles called myofibrils in the cytoplasm. Each myofibril consists of a repeating unit called sarcomere. Each sarcomere has a band of thick filaments in the middle called the A band, and they are flanked on both sides by thin filaments. One end of the thin filaments is anchored to the Z line in the I band which separates adjacent sarcomeres and the other end partially overlap the thick filaments. Due to the banded pattern provided by thin and thick filaments, skeletal muscle is also called striated muscle. The central region of the sarcomere where there is no overlap between thin and thick filaments is called the H zone. A band called the M line, in center of the H zone, link the center regions of thick filaments. Titin protein fibers from the Z line are linked to the M line and the thick filaments. Space between overlapping thick and thin filaments is bridged by projections called cross bridges from the thick filaments. In a cross-section, each thick filament is surrounded by a hexagonal array of six thin filaments and each thin filament is surrounded by a triangular array of three thick filaments. Thick filaments contain the contractile protein, myosin. Thin filaments contain the contractile protein, actin and two other proteins, troponin and tropomyosin.
Molecular mechanisms of contraction
Each actin molecule contains a binding site for myosin. Each myosin molecule contains a binding site for actin and one for ATP.
Sliding-filament mechanism
Muscle contraction is produced by cross-bridge cycles. A cycle has 4 steps:
- Energizing of myosin cross-bridge
A + M•ATP —> A + M*•ADP•Pi (ATP is energizer here) - Attachment of cross-bridge to a thin filament
A + M*•ADP•Pi —> A•M*•ADP•Pi - Movement of cross-bridge, producing tension
A•M*•ADP•Pi —> A•M + ADP + Pi - Detachment of cross-bridge from thin filament
A•M + ATP —> A + M•ATP (ATP is modulator here)
Movement of the cross-bridges make the overlapping thick and thin filaments slide past each other (they do not change in length) to produce a contraction.
Roles of troponin, tropomyosin and calcium
In a resting muscle fiber, the protein tropomyosin, held by troponin, covers the myosin-binding sites on actin and prevents cross bridges from making contact with actin. An action potential releases Ca2+ from the sarcoplasmic reticulum of the cell and increases the cytosolic concentration of Ca2+ in the muscle fiber. When Ca2+ binds to troponin, it removes tropomyosin from the myosin-binding site and makes it possible for cross bridges to attach with actin.
Sarcoplasmic reticulum
The sarcoplasmic reticulum is homologous to endoplasmic reticulum. Forms a sleeve around each myofibril. It has enlarged regions called lateral sacs that store Ca2+, and a tubular structure called transverse (T) tubule. Depolarization of the plasma membrane leads to depolarization of the T-tubule and opens the Ca2+ channels of the lateral sacs. To end contraction, Ca2+ is pumped back into the lateral sacs by active transport proteins called Ca2+-ATP-ases.
Neuromuscular junction
Nerve cells that innervate skeletal muscle fibers are called motor (somatic efferent) neurons. These neurons have cell bodies in the CNS and large, myelinated axons that can propagate action potentials at high velocities. At a muscle, the axon gives branches to many muscle fibers but each fiber gets only one branch. A motor neuron and the fibers it innervates are together called a motor unit. The region of muscle-fiber plasma membrane lying directly under the axon is called the motor endplate and the junction is called the neuromuscular junction. Axon terminals of a motor neuron contain vesicles filled with acetylcholine (ACh). An action potential opens Ca2+ channels in the nerve plasma membrane and Ca2+ diffuses in to enable these vesicles to fuse with the plasma membrane and release ACh in the extracellular space. ACh opens ion channels in the motor endplate and produces a depolarization called endplate potential (EPP). The enzyme acetylcholinesterase on the motor endplate breaks down ACh to close the ion channels and return the plate to resting potential.
Mechanics of a single fiber contraction
Force exerted on an object by a contracting muscle is called muscle tension, and the force exerted on the muscle by the object (weight) is called load. These are opposing forces and whether exertion of force leads to fiber shortening depends on relative magnitudes of tension and load. For fibers to shorten and move a load, tension must be greater than load. When a muscle develops tension but does not shorten, the contraction is called isometric (constant length). Seen when muscle supports a load in constant position or attempts to move a supported load that is greater than the tension. During such a contraction, the bound cross-bridges do not move. A contraction in which the muscle shortens while load remains constant is called isotonic (constant tension). In such a contraction, the cross-bridges bound to actin move, shortening the fibers. Before an isotonic shortening, there is a period of isometric contraction during which tension increases. A lengthening (eccentric) contraction occurs when a load on a muscle is greater than the tension and the load lengthens the muscle. Not an active process but a result of external force on the muscle. In a lengthening contraction, cross bridges are pulled toward the Z line.
Twitch contraction
Mechanical response of a single muscle fiber to a single action potential. Following the action potential, there is a latent period, before the tension in muscle fiber increases. Time interval from the beginning of tension development and peak tension is called contraction time. The latent period is longer in an isotonic twitch than in an isometric twitch while the duration of contraction is longer in an isometric twitch than in an isotonic twitch. The latent period is positively correlated while the velocity of shortening, duration of twitch and distance shortened are negatively correlated with load.
Frequency-tension relation
An increase in muscle tension from successive action potentials is called summation and a maintained contraction in response to repetitive stimulation is called tetanus. If a tetanus oscillates, it is called unfused tetanus while a tetanus without oscillations is called fused tetanus.
Length-tension relation
Passive tension in a relaxed fiber increases with increased stretch due to the elongation of titin filaments. The magnitude of active tension during contraction depends on the passive tension of a fiber because the potential for cross-bridge formation is different at different overlaps between actin and myosin filaments. The length at which the fiber develops the greatest active tension is called optimal length, l0. In a relaxed state, the length of most fibers is near l0.
Skeletal muscle energy metabolism
Muscle glycogen is the major fuel at the initial stages of exercise and is followed by the utilization of blood glucose and fatty acids.
A muscle fiber generates ATP by:
- Phosphorylation of ADP by creatine phosphate. Source of ATP during the initial phase of contraction. Followed by the slower pathways of:
- Oxidative phosphorylation in mitochondria.
- Glycolysis in cytosol. This pathway provides a majority of the energy and lactic acid is produced.
At the end of muscle activity, creatine phosphate and glycogen levels are restored by energy-dependent processes, leading to a continued elevated level of oxygen consumption, called oxygen debt, even after exercise is over.
Muscle fatigue
Decline in muscle tension as a result of previous contractile activity. A fatigued muscle also has decreased shortening velocity and slower rate of relaxation. Onset and rate of fatigue depend on the type of skeletal muscle and duration of contractile activity. If a fatigued muscle is allowed to rest, it recovers. The rate of recovery depends on the duration and intensity of the previous exercise. Fatigue is not due to low ATP since a fatigued muscle still has quite a high concentration of ATP. Fatigue may be an adaptation to prevent rigor that will result from very low ATP level. High-frequency fatigue accompanying high intensity, short-duration exercise is due to failure in the conduction of action potential in the T tubule. Recovery from such fatigue is rapid. Low-frequency fatigue seen with low intensity, long-duration exercise is due to the build-up of lactic acid, which changes the conformation of muscle proteins. Recovery from such fatigue is slow.
Types of skeletal muscle fibers
- Fast fibers contain myosin with high ATPase activity and therefore have high shortening velocity. Fatigue rapidly.
- Slow fibers contain myosin with low ATPase activity and therefore have low shortening velocity. Fatigue slowly.
- Oxidative fibers have numerous mitochondria and therefore a high capacity of oxidative phosphorylation. ATP production is dependent on bloodborne oxygen and fuel.
It also contains an oxygen-binding protein called myoglobin, which increases the rate of oxygen diffusion into the fiber. This protein gives the fibers a red color and therefore these fibers are also called red muscle fibers. Glycolytic fibers have few mitochondria but a high concentration of glycolytic enzymes and glycogen. Have a pale color and therefore are also called white muscle fibers. Larger and have more thick and thin filaments and therefore can develop more tension. Fatigue rapidly.
Three types of skeletal fibers: (l) Slow-oxidative fibers, (2) Fast-oxidative fibers and (3) Fast-glycolytic fibers. Most muscles contain all three kinds of fibers.
Control of muscle tension
Total tension a muscle can develop depends on:
- Amount of tension developed by each fiber
- Number of fibers contracting at any time, which in turn depends on: (a) Number of fibers in each motor unit (motor unit size) and (b) Number of active motor units. Increasing the number of active motor units in a muscle, called recruitment, is achieved by increasing excitatory input to the motor neurons. Finer control of muscle tension is possible in muscles with small motor unit size.
Muscle adaptation to exercise
Increased amount of contractile activity (exercise) increases size (hypertrophy) of muscle fibers and capacity for ATP production. Low-intensity exercise affects oxidative fibers, increasing the number of mitochondria and capillaries. High-intensity exercise affects glycolytic fibers, increasing their diameter by an increased synthesis of actin and myosin filaments, and an increased synthesis of glycolytic enzymes.
Lever action of muscles and bones
A contracting muscle exerts a pulling force and moves the bones. If this leads to a limb bending at a joint, it is called flexion while if it leads to a limb straightening from a joint, it is called extension. Groups of muscles producing opposite movements at a joint are called antagonists.
Skeletal muscle disease
Poliomyelitis leads to paralysis of skeletal muscles due to destruction of motor neurons by a virus. Muscular dystrophy is a progressive degeneration of skeletal and cardiac muscle fibers due to a low amount of the protein dystrophin that maintains the structural integrity of the plasma membrane during stretching. It is a sex-linked recessive disease. Myastheniagravis leads to muscle fatigue due to low number of ACh receptors on the motor endplate.
Smooth Muscle
A smooth muscle lacks the banded structure of skeletal muscles. Controlled by the autonomic nervous system and is not under voluntary control.
Structure
A smooth muscle fiber is a spindle-shaped, uninucleate cell. Has the capacity to divide throughout life. The thick and thin filaments are not regularly aligned into sarcomeres but are oriented diagonally to the long axis of the cell. Thin filaments are attached to the plasma membrane or to cytoplasmic structures called dense bodies. The concentration of myosin is low and that of actin is high.
Contraction
Thin filaments do not have troponin. As cytosolic Ca2+ concentration increases,
- Calcium binds to calmodulin, a protein
- Calcium-calmodulin complex binds to the enzyme, myosin light-chain kinase and activates it
- The active kinase uses ATP to phosphorylate the myosin cross-bridges
- The phosphorylated cross-bridges bind to actin
- Myosin is dephosphorylated by myosin light-chain phosphatase
ATPase activity is low and therefore cross-bridge cycling and muscle shortening is slow. Dissociation of dephosphorylated cross-bridges is slow and therefore the muscle can maintain tension with very low ATP consumption. Does not undergo fatigue during prolonged periods of activity. The range of muscle lengths over which tension can be developed is greater.
Sources of cytosolic calcium
- Sarcoplasmic reticulum – Does not have T-tubules.
- Extracellular calcium – Opening of Ca2+ channels in the plasma membrane.
Rate of Ca2+ removal is slower with the result that a twitch lasts longer. Concentration of Ca2+ in response to a single action potential is only sufficient enough to activate a proportion of cross-bridges. Therefore, tension in smooth muscle can be graded by varying cytosolic Ca2+ concentration. A low-level tension is always maintained, even in the absence of external stimuli, and this is called a smooth-muscle tone.
Membrane activation
The plasma membrane of smooth muscles receives both excitatory and inhibitory inputs and the contractile state of the muscle depends on the relative intensity of both. Some smooth muscle fibers generate action potentials spontaneously in the absence of any input. The potential change occurring during such spontaneous depolarization is called pacemaker potential. Smooth muscles do not have motor endplates. The postganglionic autonomic neuron divides into branches in the smooth muscle fibers, and each branch has a series of swollen regions called varicosities, which contain vesicles filled with neurotransmitter that is released when an action potential arrives. The same neurotransmitter can produce excitation in one fiber and inhibition in the other. Varicosities from a single axon may innervate several fibers and a single fiber may receive varicosities from both sympathetic and parasympathetic neurons.
Smooth muscle plasma membrane also binds hormones and respond to them. Paracrine agents, acidity, oxygen concentration, osmolarity, ion composition can also influence smooth muscle tension, providing a response mechanism to local factors.
(1) Single-unit Smooth Muscle
All the fibers undergo synchronous activity because adjacent fibers arc linked by gap junction d action potential occurring anywhere is propagated to all other cells. The whole muscle responds to stimulation as a single unit. Some of the fibers may be pacemaker cells and they can control the contraction of the entire muscle a majority of which may consist of non-pacemaker cells. The nerve terminals, therefore, need to be restricted only to the pacemaker cells.
(2) Multi-unit Smooth Muscle
Each fiber responds independently of its neighboring fibers because there are no connecting gap junctions.
You will also like...

Kidneys and Regulation of Water and Inorganic Ions
The kidneys are responsible for the regulation of water and inorganic ions. Read this tutorial to learn about the differ..

The Evolution of Cell Organelles
The nucleus containing the genetic material, DNA, and the mitochondria, well-identified as the "powerhouse of the cell",..

Human Reproduction and Fertilization
For human species to obviate extinction, reproductive mature adults should be producing viable offspring in order to con..

Still Freshwater & Plants
Plants in lentic habitats have features not found in terrestrial plants. They acquired these features as they adapt to t..

Muscle
Muscle cells are specialized to generate force and movement. Learn about the different types of muscle tissues in this t..
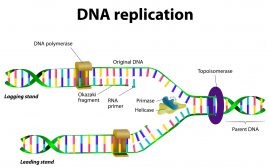
DNA Structure & DNA Replication
DNA is a double helix structure comprised of nucleotides. A nucleotide, in turn, is made up of phosphate molecule, deoxy..
