Respiration
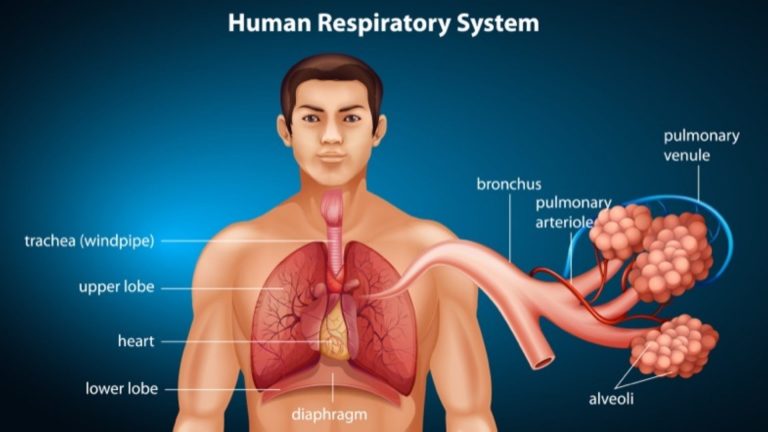
The human respiratory system
Table of Contents
Organization of the Respiratory System
Each lung is composed of air sacs called alveoli – the sites of gas exchange with the blood. Airways are tubes through which air flows between the external environment and alveoli. A respiratory cycle consists of an inspiration (inhalation) movement of air from the external environment into alveoli, and expiration (exhalation) – the movement of air from alveoli to the external environment.
Airways and blood vessels
During inspiration, air passes through nose/mouth, pharynx (throat), and larynx. These constitute the upper airways. Airways beyond the larynx are divided into 2 zones:
- The conducting zone where there is no gas exchange. This consists of the tracheal tube, which branches into two bronchi. Each of them enters each lung and makes further branching. Walls of trachea and bronchi contain cartilage for support. The first branches without cartilage are called terminal bronchioles.
- The respiratory zone where gas exchange occurs. Consists of respiratory bronchioles with alveoli attached to them.
Epithelial surfaces of airways up to respiratory bronchioles have cells that secrete mucus to trap particulate matter in the air, which is then moved by cilia present on these cells and swallowed. Macrophages, which engulf pathogens, are also present.
Alveoli: the site of gas exchange
Alveoli are hollow sacs having open ends continuous with lumens of airways. Inner walls lined by a single layer of flat epithelial cells called type I alveolar cells, interspersed by thicker, specialized cells called type II alveolar cells. Alveolar walls contain capillaries and a small interstitial space with interstitial fluid and connective tissue. Blood within an alveolar wall capillary is separated from the air within alveolus by a very thin barrier. There are also pores in the walls that permit the flow of air. The extensive surface area and the thin barrier permit the rapid exchange of large quantities of oxygen and carbon dioxide by diffusion.
Lungs and the thoracic wall
Lungs are situated in thorax, i.e. the body compartment between the neck and abdomen. Thorax is a closed compartment, bound at the neck by muscles, and separated from the abdomen by a sheet of skeletal muscle, the diaphragm. The wall of the thorax is composed of ribs, breastbone (sternum), and intercostal muscles between ribs.
A closed sac, the pleural sac, consisting of a thin sheet of cells, called pleura, surrounds each lung. The pleural surface coating the lung (visceral pleura) is attached to the lung by connective tissue. The outer layer (parietal pleura) is attached to the thoracic wall and diaphragm. A thin layer of intrapleural fluid separates the two layers of pleura. Changes in hydrostatic pressure of the intrapleural fluid – the intrapleural pressure (Pip) or the intrathoracic pressure cause lungs and thoracic wall to move in and together during breathing.
Ventilation and Lung Mechanics
Ventilation is the exchange of air between the atmosphere and the alveoli. Air moves by bulk flow — from the region with high pressure to the region with low pressure. Flow rate can be found with:
F = (Patm – Palv)/R
where, Patm, is the atmospheric pressure and Palv is the alveolar pressure.
During ventilation, the air is moved in and out of the lungs by changing alveolar pressure through changes in lung dimensions.
The volume of lungs depends on (1) difference in pressure between inside and outside of the lungs, called transpulmonary pressure and (2) stretchability of the lungs, called lung compliance.
Muscles used in respiration are attached to the chest wall. When they contract or relax, they change the chest dimensions. This changes transpulmonary pressure, which, in turn, changes lung volume. This changes alveolar pressure, causing air to flow in or out of the lungs.
Stable Balance Between Breaths
Transpulmonary pressure = Palv – Pip
Palv is zero, which means it is the same as atmospheric pressure. Pip is negative or less than atmospheric pressure. The elastic recoil of the lung inwards and the elastic recoil of the chest wall outwards will increase the volume of intrapleural space between them and decrease the pressure within. Therefore, transpulmonary pressure is greater than zero. This pressure puts an expanding force equal to the force of elastic recoil of the lung and keeps it from collapsing. The volume of lungs is kept stable and there is air inside the lungs. By a similar phenomenon, the pressure difference across the chest (Patm- Pip) directed inward keeps the elastic chest wall from moving outward excessively.
Inspiration
Inspiration is initiated by neurally induced contractions. The diaphragm moves down and intercostal muscles move rib cage out. The size of the thorax increases and Pip drops even further. This increases transpulmonary pressure, thus expanding the lungs. This increases the size of alveoli, decreasing pressure within them. When Patmalv, it causes a bulk flow of air from the external environment through airways and into the lungs. When Patm = Palv, airflow ceases.
Expiration
The diaphragm and intercostal muscles relax during expiration. The chest recoils, becoming smaller. Pip increases, thus decreasing transpulmonary pressure. Lungs recoil, compressing air in alveoli and increasing Palv. Air passively flows out from alveoli to the external environment. Under certain conditions, air can also be expired actively by contracting a set of intercostal and abdominal muscles that decrease thoracic dimensions.
Lung Compliance
Lung compliance is a measure of elasticity or the magnitude of change in lung volume (ΔVL) that can be produced by a given change in transpulmonary pressure.
CL = ΔVL / Δ (Palv – Pip)
When lung compliance is low, Pip must be made lower to achieve lung expansion. This requires more vigorous contractions of the diaphragm and intercostal muscles.
Determinants of lung compliance
Since the surface of alveolar cells is moist, surface tension between water molecules resists stretching of lung tissue. Type II alveolar cells secrete a substance called pulmonary surfactant that decreases surface tension and increases lung compliance. Respiratory distress syndrome of newborns is a result of low lung compliance.
Airway Resistance
Resistance is determined mainly by radius. Transpulmonary pressure exerts a distending force and keeps airways from collapsing, makes them larger during expiration and smaller during inspiration. Asthma is a disease in which airway smooth muscle contracts and increases airway resistance.
Chronic Obstructive Pulmonary Disease (COPD) is chronic bronchitis or the production of excessive mucus in bronchi that obstructs the airways.
Heimlich Maneuver
This maneuver is the manual application of an upward pressure applied to the abdomen of a person who is choking on an object caught in the airways. This maneuver can force the diaphragm to move up, reducing the thoracic size, and increasing alveolar pressure. The forceful expiration that is produced can expel the lodged object.
Lung Volumes and Capacities
Tidal volume is the volume of air entering the lungs during a single inspiration or leaving the lungs in a single expiration. The maximal amount of air that can be increased ABOVE this value during the deepest inspiration is called inspiratory reserve volume. After the expiration of a resting tidal volume, the volume of air still remaining in the lungs is called functional residual capacity. The additional volume of air that can be expired (by active contraction of expiratory muscles) after the expiration of resting tidal volume is called expiratory reserve volume. Air still remaining in the lungs after a maximal expiration is called residual volume. Vital capacity is the maximal volume of air that can be expired after a maximal inspiration.
Alveolar Ventilation
Minute ventilation = Tidal volume x Respiratory rate
Units: (ml/min) = (ml/breath) x (breaths/minute)
Anatomic dead space is the space within the airways that does not permit gas exchange with the blood. The total volume of fresh air entering the alveoli per minute is called alveolar ventilation.
Ventilation = (Tidal volume – anatomic dead space) x respiratory rate
Units: (ml/min) = (ml/breath) – (ml/breath) x (breaths/min)
Since a fixed volume of each tidal volume goes to dead space, increased depth of breathing is more effective in elevating alveolar ventilation than increased breathing rate. The volume of inspired air that is not used for gas exchange as a result of reaching alveoli with no blood supply is called alveolar dead space. The sum of anatomic and alveolar dead space is called physiologic dead space.
Gas Exchange in Alveoli and Tissues
In steady-state, the volume of oxygen consumed by body cells per unit time is equal to the volume of oxygen added to the blood in the lungs, and the volume of carbon dioxide produced by cells is. identical to the rate at which it is expired. The ratio of CO2 produced / O2 consumed is called respiratory quotient (RQ), which depends on the type of nutrients being used for energy.
Alveolar Gas Pressures
Alveolar P02 is lower than atmospheric P02 because oxygen in alveolar air keeps entering pulmonary capillaries. Alveolar Pool is higher than atmospheric PCO2 because carbon dioxide enters alveoli from pulmonary capillaries. P02 is positively correlated with: (1) PO2, of atmospheric air, (2) rate of alveolar ventilation and inversely correlated with, and (3) rate of oxygen consumption. PCO2 is inversely correlated with (1) the rate of alveolar ventilation and (2) positively correlated with the rate of oxygen consumption.
Hypoventilation is an increase in the ratio of carbon dioxide production to alveolar ventilation whereas hyperventilation is a decrease in this ratio.
Alveolar-Blood Gas Exchange
Blood entering pulmonary capillaries is systemic venous blood having a high PCO2 and a low P02. Differences in partial pressures of oxygen and carbon dioxide on two sides of the alveolar-capillary membrane result in net diffusion of oxygen from alveoli to blood and of carbon dioxide from the blood to alveoli. With this diffusion, capillary blood P02 rises and its PCO2 falls and net diffusion of these gases ceases when capillary partial pressures become equal to those in alveoli.
In diffuse interstitial fibrosis, alveolar walls thicken with connective tissue reducing gas exchange. Ventilation-perfusion inequality can result from: (1) ventilated alveoli with no blood supply and (2) blood flow through alveoli with no ventilation, reducing gas exchange.
Gas Exchange in Tissues
Metabolic reactions within cells consume oxygen and produce carbon dioxide. Intracellular PO2 is lower and PCO2 is higher than in blood. As a result, there is a net diffusion of oxygen from the blood into cells, and a net diffusion of carbon dioxide from cells into the blood.
Transport of Oxygen in Blood
Oxygen is carried in 2 forms: (1) dissolved in plasma and (2) reversibly combined with hemoglobin (Hb) molecules in erythrocytes. Each Hb molecule is a globin protein with four iron-containing heme groups attached to it. Each heme group binds one molecule of oxygen. Hb exists in two forms: deoxyhemoglobin (Hb) and oxyhemoglobin (HbO2). The fraction of all Hb in form of Hb02 is called percent Hb saturation.
Percent saturation = (O2 bound to Hb x 100)/ Maximal capacity of Hb to bind O2 (Oxygen carrying capacity)
Effect of pO2 on Hemoglobin Saturation
Raising blood pO2 increases the combination of oxygen with Hb and binding of one oxygen molecule to Hb increases the affinity of the remaining sites on the same molecule. Therefore, the extent to which oxygen combines with Hb increases rapidly as pO2 increases and this relationship between the two variables is called the oxygen-hemoglobin dissociation curve. The plateau of the curve at higher pO2 provides a safety factor for oxygen supply at low alveolar pO2.
The diffusion gradient favoring oxygen movement from alveoli to blood is maintained because oxygen binds to Hb and keeps the plasma PO2, low and only dissolved oxygen contributes to pO2. In tissues, the procedure is reversed.
Carbon Monoxide (CO) and Oxygen Carriage. CO competes for the oxygen binding sites on Hb and also decreases the unbinding of oxygen from Hb.
Effects of Blood PC02, H+ concentration, Temperature, and DPG on Hb Saturation. The more active a tissue is, the greater is its pCO2, H+ concentration, and temperature. CO2, H+ ions, and DPG (2, 3-diphosphoglycerate) combine with Hb and modify it allosterically, thereby shifting the dissociation curve to the right. This shift causes Hb to release more oxygen to the tissues.
Transport of Carbon Dioxide in Blood
Some fraction of carbon dioxide is dissolved and carried in the blood. Some react reversibly with Hb to form carbamino Hb.
CO2 + Hb ↔ HbC02
Some carbon dioxide is converted to bicarbonate.
CO2 + H2O ↔ H2CO3 ↔ HCO3– + H+
(by carbonic anhydrase)
The enzyme, carbonic anhydrase, is present in erythrocytes where the reaction takes place after which the bicarbonate moves out into the plasma.
Transport of H+ Ions Between Tissues and Lungs
If a person is hypoventilating, arterial H+ concentration rises due to increased pCO2 and this is called respiratory acidosis. Hyperventilation lowers H+ and this is called respiratory alkalosis. Deoxyhemoglobin has a higher affinity for H+ ions than oxy-hemoglobin and binds most of H+ produced. In the lungs, when deoxyhemoglobin is converted to oxyhemoglobin, H+ ions are released.
Control of Respiration
Diaphragm and intercostal muscles are skeletal muscles and therefore breathing depends upon the cyclical excitation of these muscles. Control of this neural activity resides in neurons called medullary inspiratory neurons in medulla oblongata. These neurons receive inputs from apneustic and pneumotaxics center in pons. Negative feedback from pulmonary stretch receptors is also involved in controlling respiration (Hering Breur reflex).
Control of Ventilation
- Control by pO2 and pC02. Peripheral chemoreceptors called carotid bodies and aortic bodies are in close contact with arterial blood and are stimulated by a steep decrease in arterial PO2 and an increase in H+ concentration. They give inputs to the medulla.
- Control by H+ not due to CO2. Lactic acid in exercising muscles can cause metabolic acidosis or metabolic alkalosis, changing H+ concentration and stimulating peripheral chemoreceptors.
- Control of Ventilation during Exercise. Blood pCO2, pO2, and H+ concentration due to CO2 do no change much during exercise due to compensatory hyperventilation. Change in H+ concentration due to lactic acid, input from mechanoreceptors in joints and muscles, increase in body temperature, increase in plasma epinephrine, etc. play important roles in stimulating ventilation.
Protective Reflexes
As for other ventilatory responses, protective reflexes (such as cough and sneeze reflexes) protect the respiratory system from irritants. Receptors for sneeze located in nose or pharynx, while those for cough are located in the larynx, trachea, and bronchi. The reflexes are characterized by a deep inspiration followed by a violent expiration. Voluntary control of breathing is accomplished by descending pathways from the cerebral cortex. It cannot be maintained when involuntary stimuli are very high. Reflex from J receptors, which are located in the lungs, is stimulated by an increase in lung interstitial pressure due to occlusion of a pulmonary vessel (pulmonary embolus), left ventricle failure, etc. The reflex effect is tachypnea (rapid breathing).
Hypoxia
Hypoxia is the deficiency of oxygen at the tissue level. There are four types:
- Hypoxic hypoxia (hypoxemia) which is characterized by reduced arterial PO2.
- Anemic hypoxia occurs when the total oxygen content of blood is reduced due to the inadequate number of erythrocytes, deficient or abnormal Hb, or binding of CO to Hb. Arterial PO2 remains normal.
- Ischemic hypoxia (hypoperfusion hypoxia) occurs when blood flow to tissues is low.
- Histotoxic hypoxia occurs when tissue is unable to utilize the oxygen due to interference from a toxic agent. However, the quantity of oxygen reaching the tissue is normal.
The retention of carbon dioxide and increased arterial pCO2 is called hypercapnia.
Emphysema
Emphysema is the disease characterized by increased airway resistance, the decreased surface area for ventilation due to alveolar fusion, and ventilation-perfusion inequalities.
Nonrespiratory Functions of the Lungs
Lungs (1) concentrate a large number of biologically active substances in the bloodstream and also remove them, (2) produce and add new substances to blood, and (3) trap and dissolve small blood clots.
You will also like...
The Human Nervous System
The nervous system is essentially a biological information highway. This tutorial gives an overview of the nervous syste..
Biological Cell Introduction
It only takes one biological cell to create an organism. A single cell is able to keep itself functional through its 'mi..
Physiological Homeostasis
Homeostasis is essential to maintain conditions within the tolerable limits. Otherwise, the body will fail to function p..

Abiotic and Biotic Factors
This tutorial deals with the abiotic factors of the freshwater environment that determine what sort of life would be sui..

Running Water Freshwater Communities
This tutorial introduces flowing water communities, which bring new and dithering factors into the equation for possible..

Origins of Life on Earth
Earth was created around 4.5 billion years ago and life began not long after. Primitive life likely possessed the elemen..
